This is the case of a late-middle-aged man who died of respiratory failure. He had the clinical diagnosis of idiopathic pulmonary fibrosis. To remind you, idiopathic pulmonary fibrosis is a clinical diagnosis, while the *pathologic* finding is usually so-called “usual interstitial pneumonia.”
The first thing that hit me when I was performing this autopsy was that the decedent’s lungs had both the look and certainly the feel of a cirrhotic liver. They were very heavy, rock solid, and had that cobblestone feel that we are all familiar with when palpating an alcoholic liver. Here are some gross photos. You can see the fibrotic nodules:
There are all sorts of different kinds of interstitial pneumonias, or else nobody could write board questions. The “usual interstitial pneumonia” is the one you use when the obvious things are ruled out. The common diagnostic criteria are:
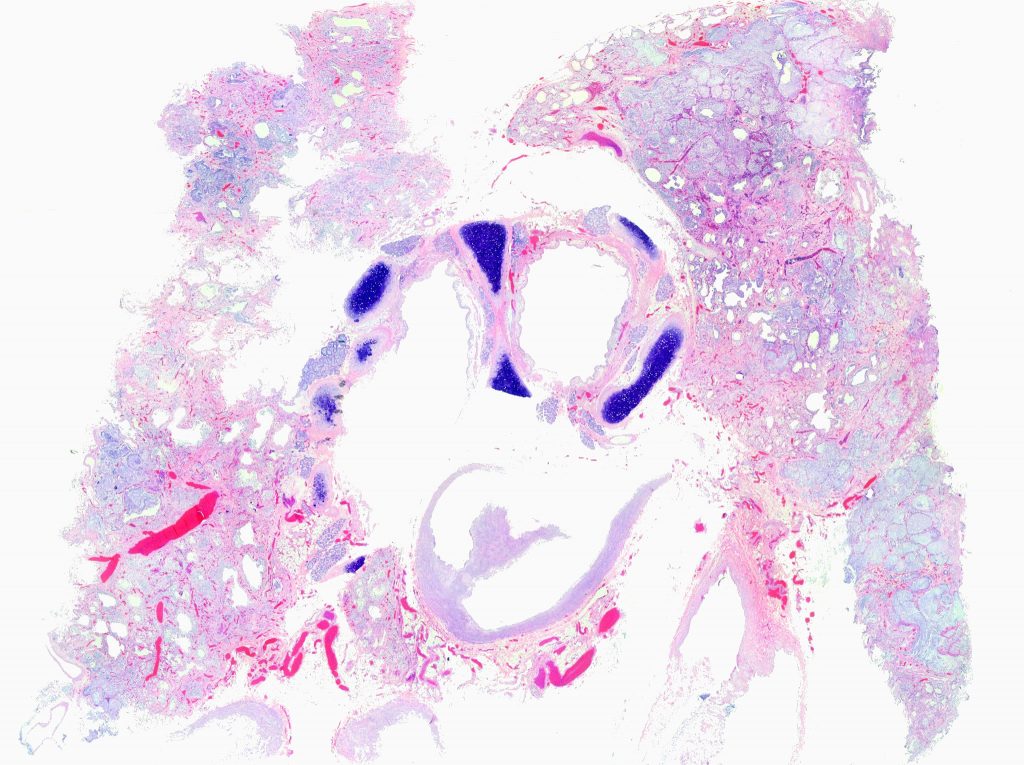
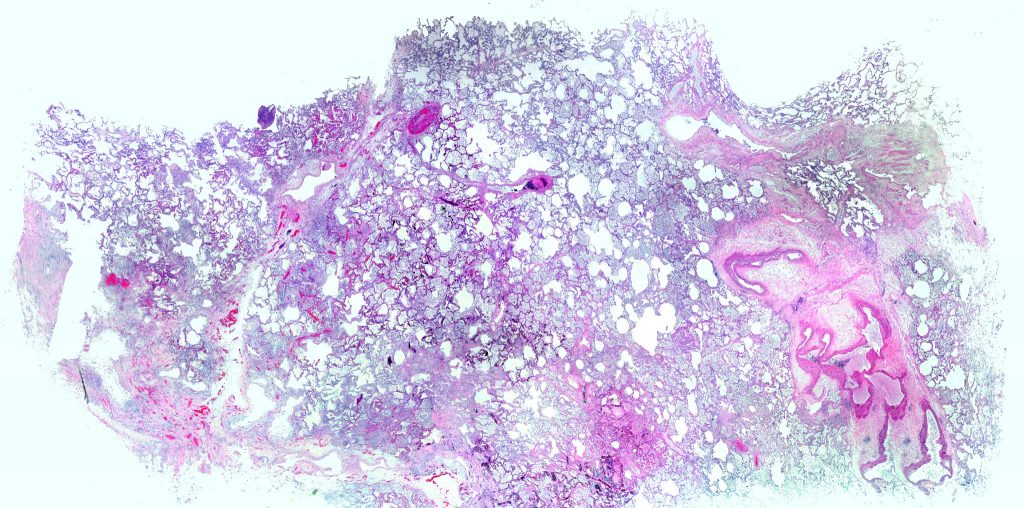
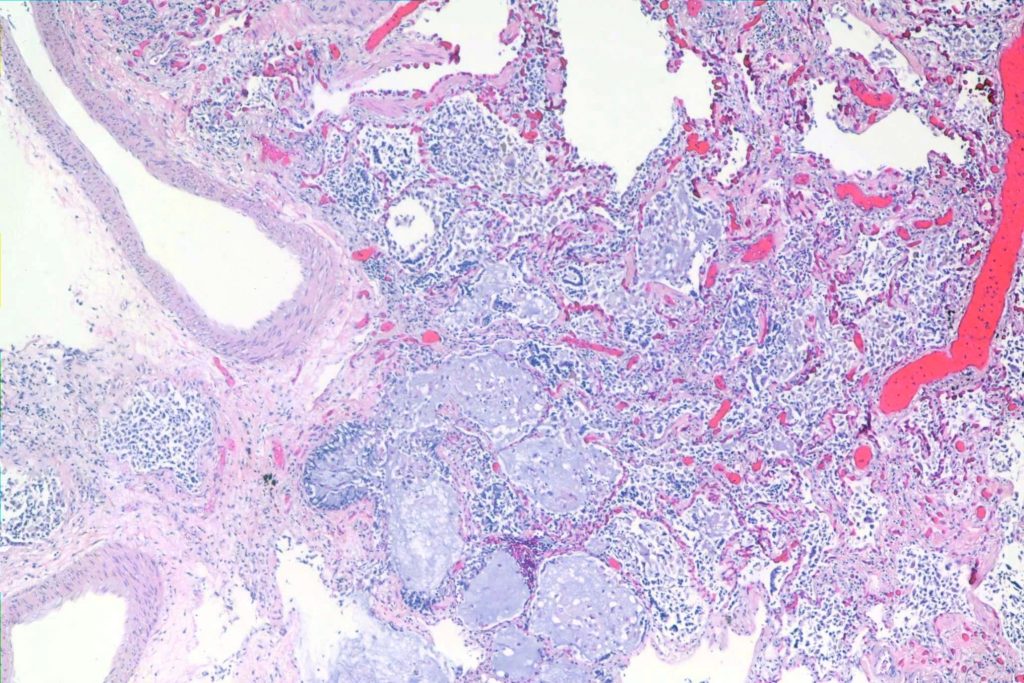
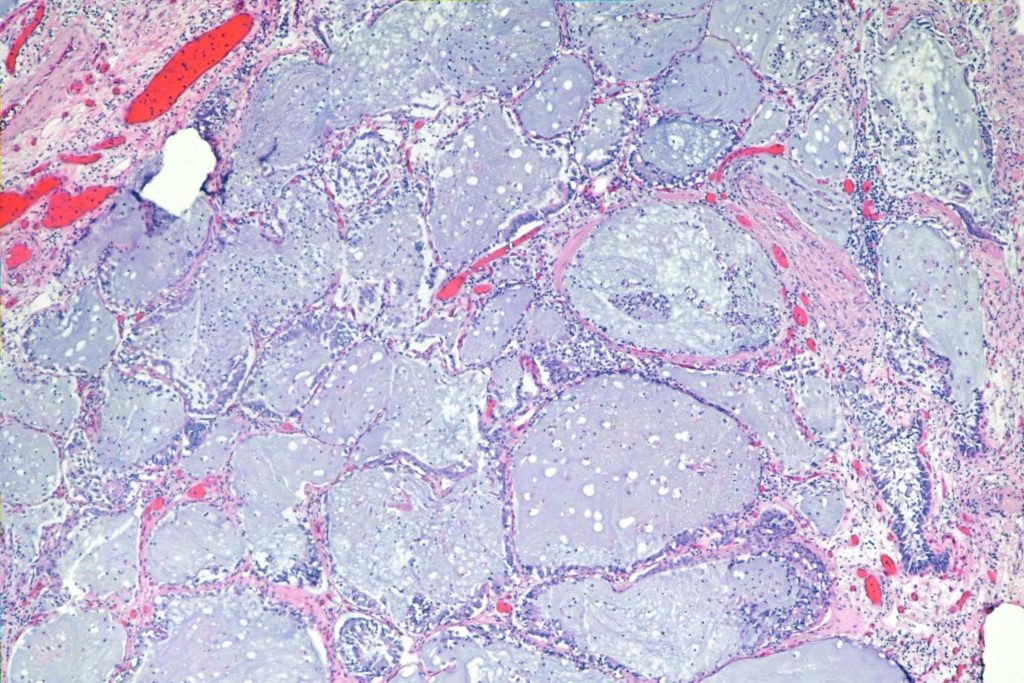
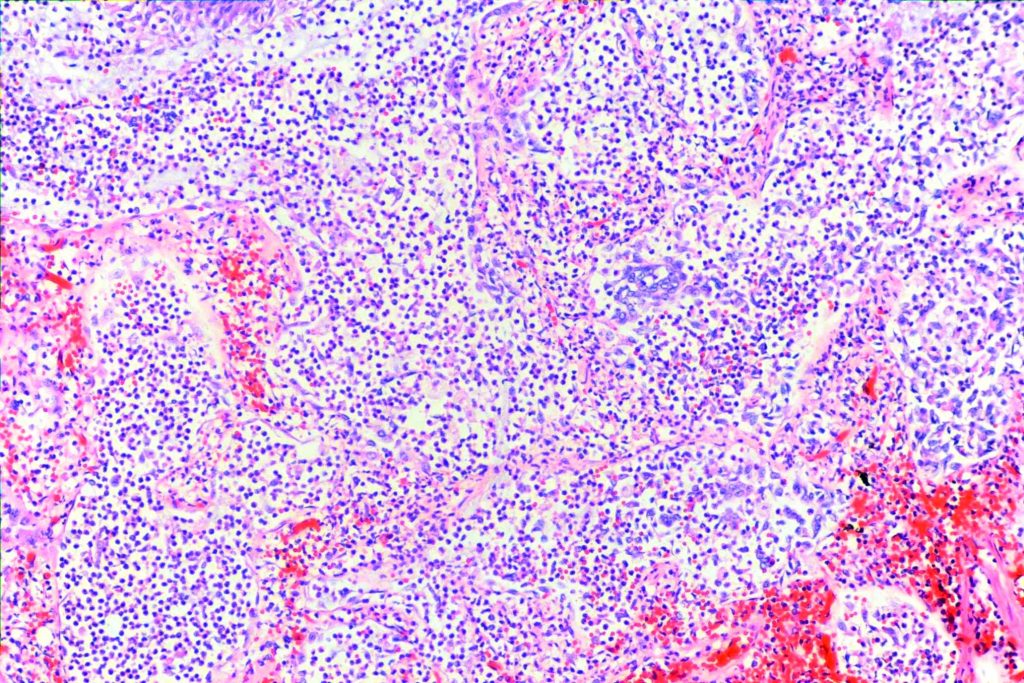
- It’s kind of patchy, so you can see “normal” places intermixed with bad fibrotic places. Here are two very low power shots of this case. There were some problems with fixing the background on the panorama shots, so I apologize for that. Nonetheless, you can see patches of relatively normal alveoli here and there. Since this was a fatal case, there weren’t all that many. Fibrosis is supposed to be at the periphery of the lobule, so you’ll see relatively normal alveoli in a patch surrounded by fibrosis. In addition, there should be distortion of the architecture of the lung.
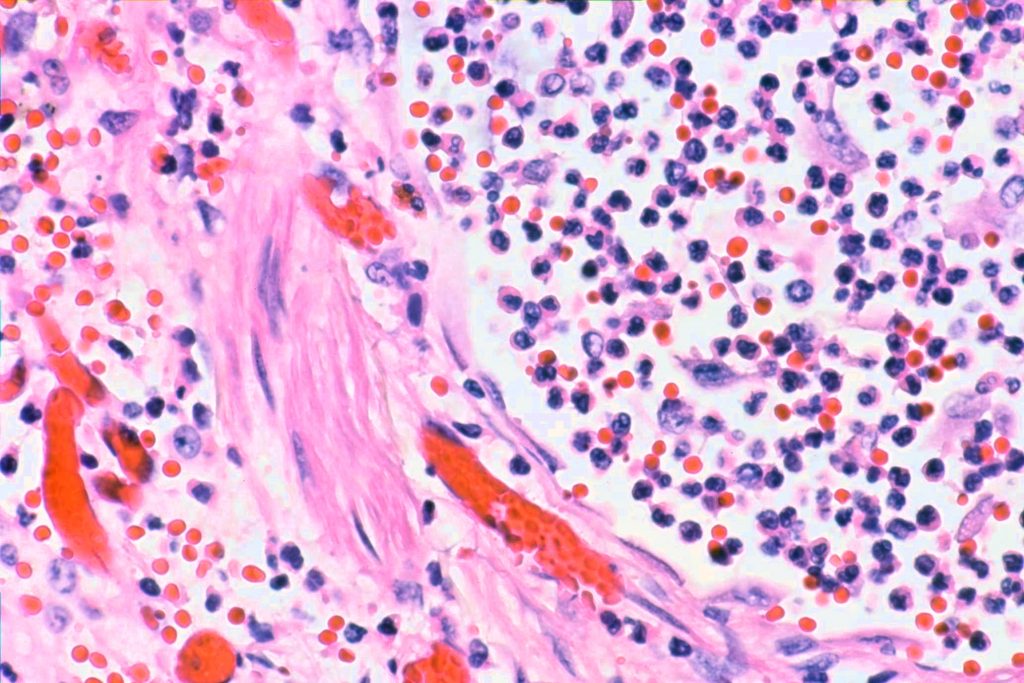
2. There should be foci of fibroblast proliferation, called, not surprisingly “fibroblast foci” in the literature. They are little lumps of fibroblasts, with the lumps usually flat on one side and rounded on the other.
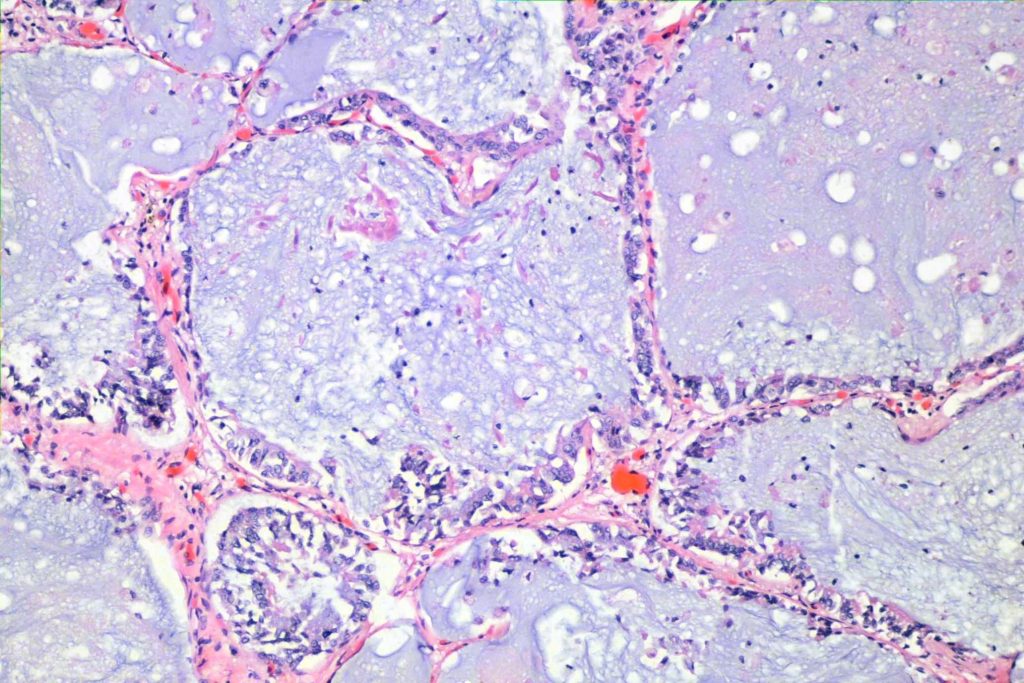
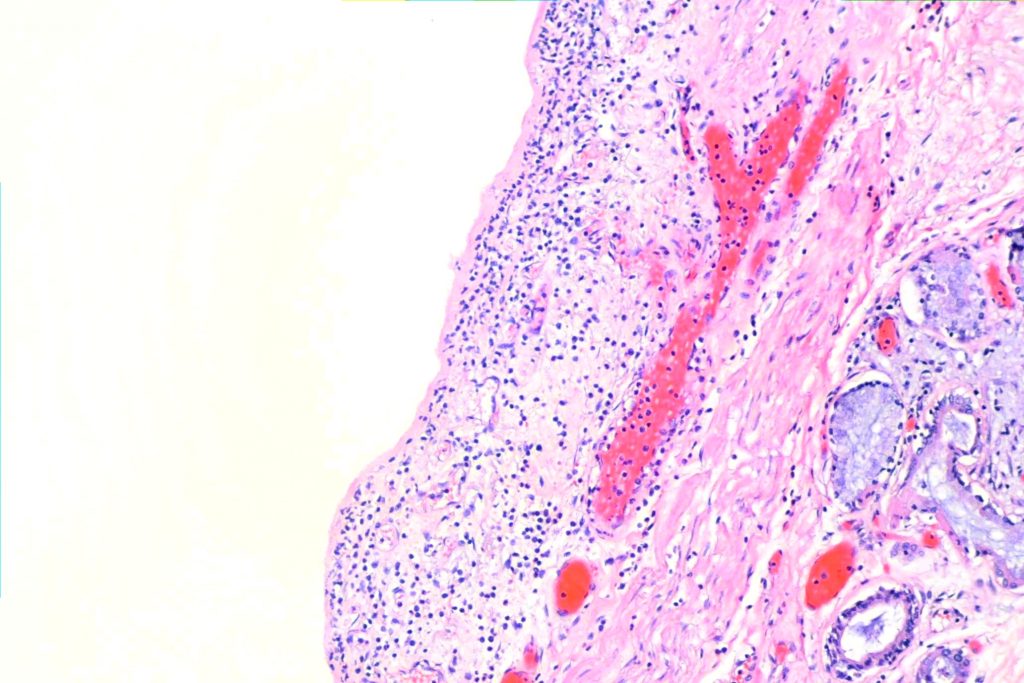
3. While honeycomb change is a common end-stage pathway for interstitial disease, and is thus fairly nonspecific, you can find it, and it helps rule out stuff that doesn’t have honeycombing. Often the spaces are lined by respiratory epithelium (“bronchiolar metaplasia”) and can be filled with mucous.
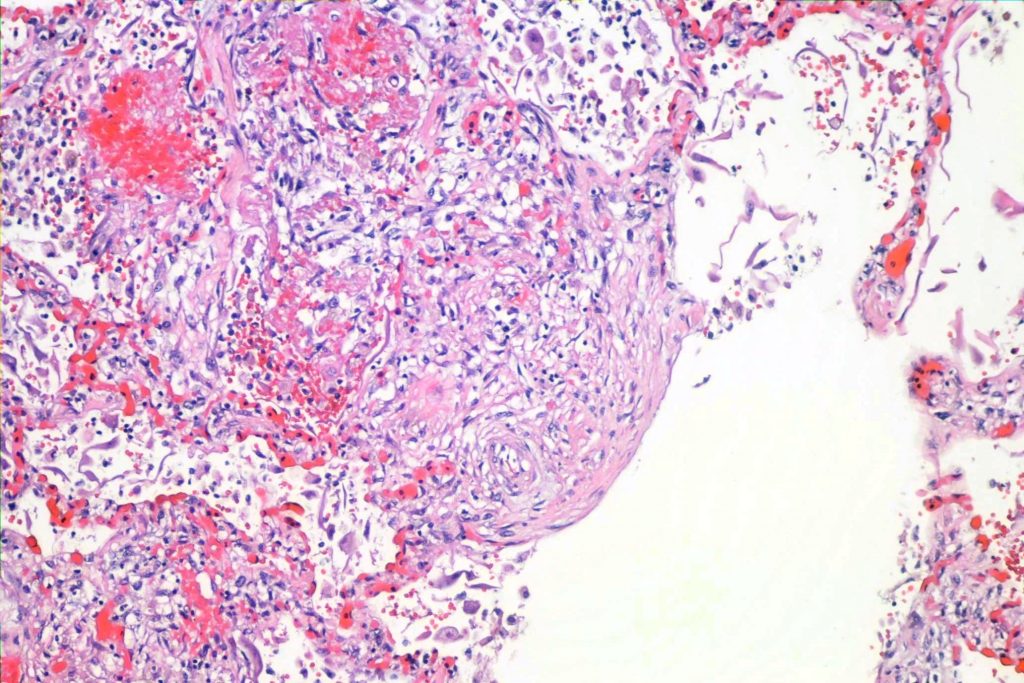
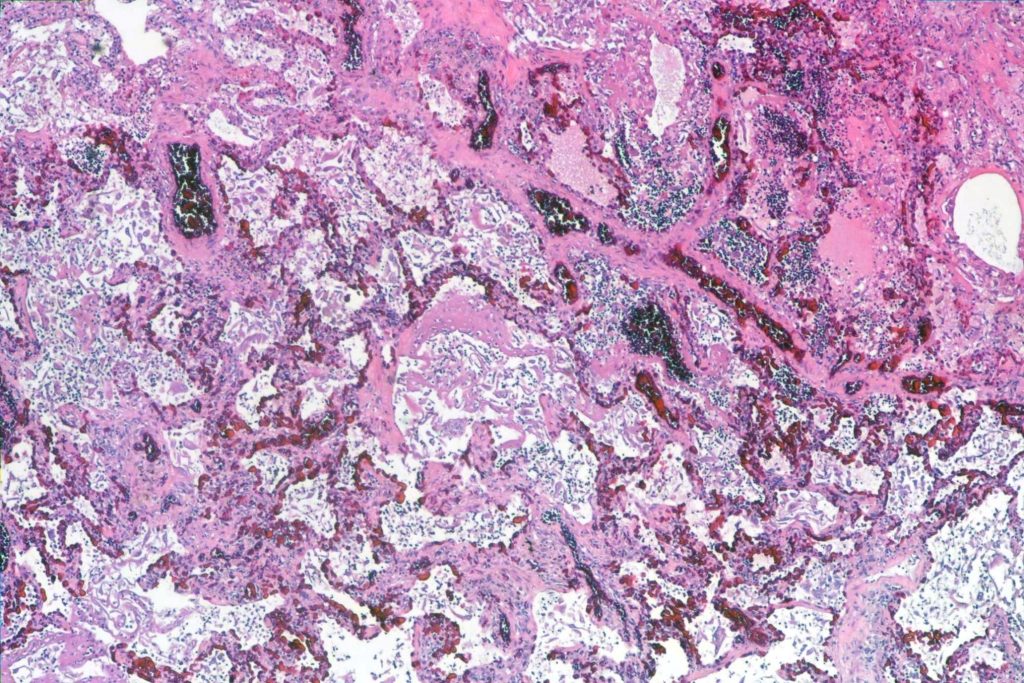
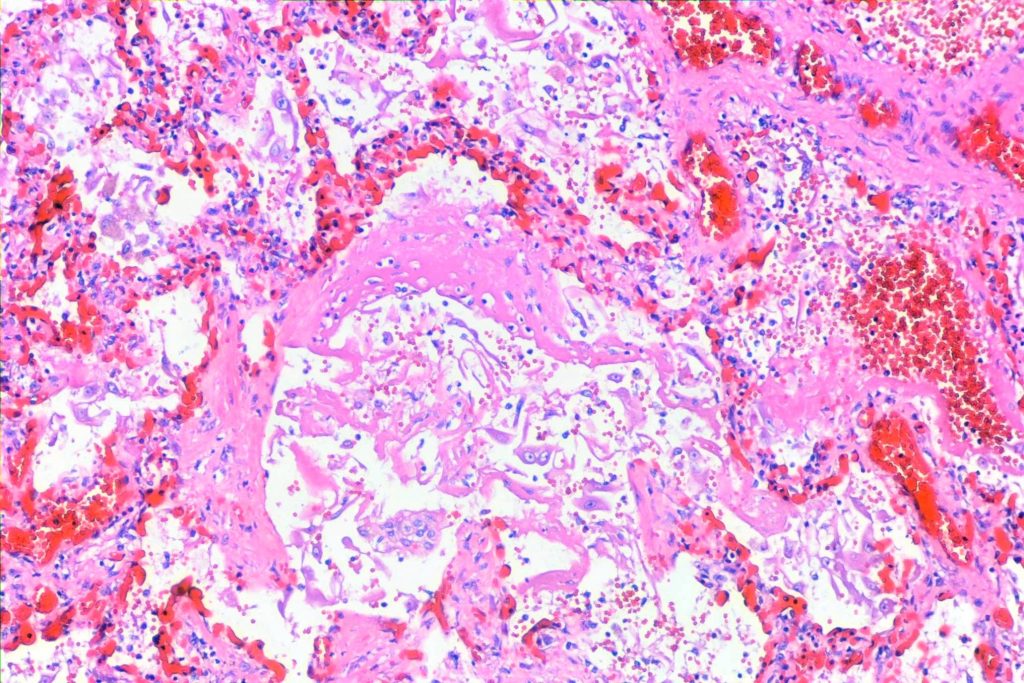
3. Some articles say that you can have some places that look like diffuse alveolar damage with hyaline membranes. Those were present in this case as well:
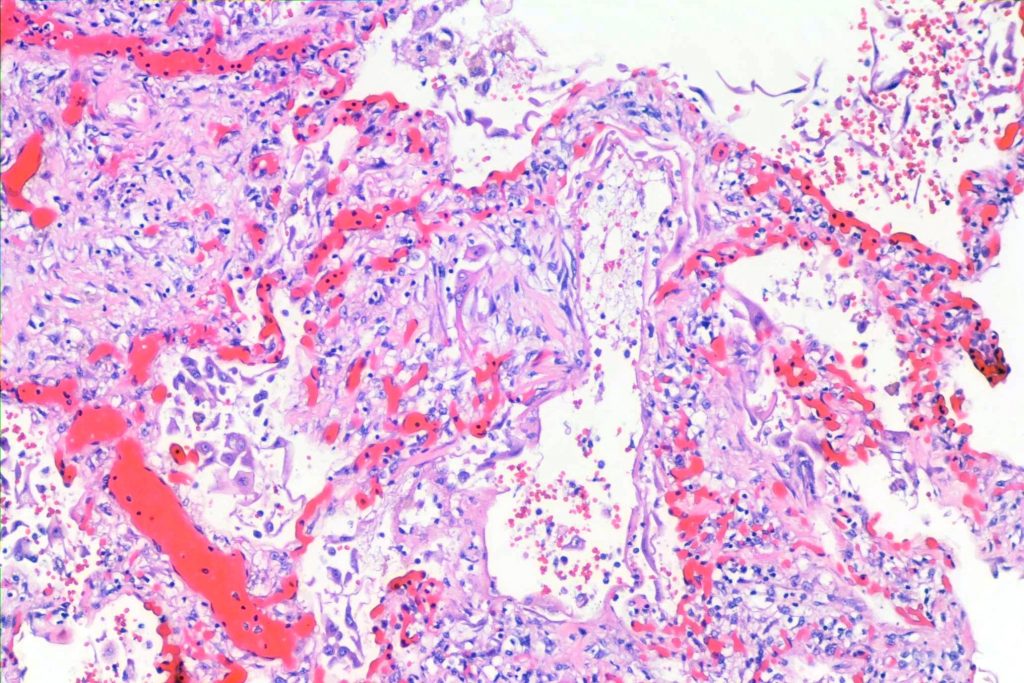
In this case there was a brochopneumonia as well. The decedent had been under terminal sedation for a few days:
And an associated acute bronchitis:
As important, you don’t have the stuff for other diagnoses. You don’t have microgranuloma for hypersensitivity pneumonitis (and other granulomatous processes). You don’t have the lymphocytic aggregates and inflammation for a connective tissue disease thing. You don’t have *just* honeycomb lung as after some insult years ago. With nonspecific interstitial pneumonia, you don’t get honeycombing.
I find it all a little confusing, but that’s how I read this case. The most impressive thing to me, though, was not the histology. It was how the lungs felt in my hands. As a forensic pathologist, I don’t see many of these very advanced terminal interstitial processes. It was impressive.