In the past month or so, I’ve had two cases of sarcoidosis, one diagnosed antemortem and one unsuspected. Both died of drug intoxication — methamphetamine and para-fluorofentanyl for one, and fentanyl and alcohol for the other.
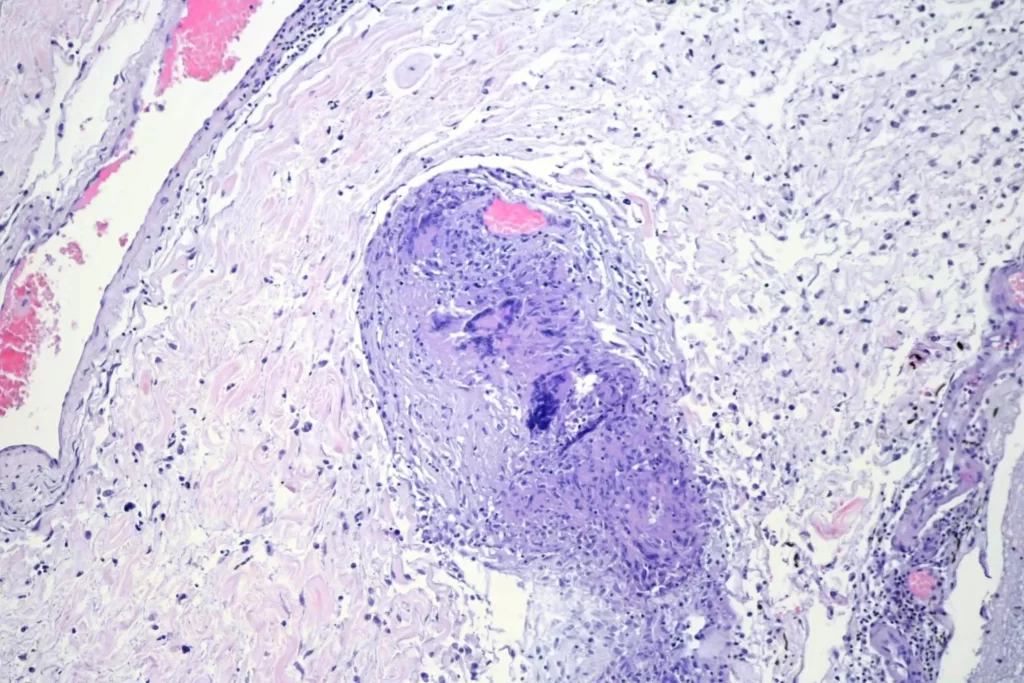
For any non-physicians who happen to be reading this, sarcoidosis is a disease of “granulomatous” inflammation. Granulomas (single “granuloma” plural “granulomas” or “granulomata”) are little balls of inflammatory tissue created by macrophages who attempt to wall off some offending substance. Normally, macrophages — some of the garbage collection cells of the body — clear out bad stuff by engulfing it and then transporting it away. When they can’t do that, sometimes they try to just wall it off, so it can’t cause problems. They collect together and form little balls around whatever it is that they don’t like. Sometimes the macrophages fuse together to become multinucleated “giant” cells. A lot of things can cause this to happen. In my practice the more common are foreign material such as debris from injected drugs, bacteria such as tuberculosis, and fungi such as histoplasmosis. Granulomata can also form as a nonspecific drug reaction. Finally, there are some autoimmune diseases or diseases where there’s some hidden trigger of an inappropriate immune reaction. The most common of these is “sarcoidosis” where you get granulomata forming for no good reason in multiple tissues.
It’s important to work up the cause of granulomatous disease if it’s symptomatic. I had an unfortunate case some years ago in another state of a young woman who died of “sarcoidosis.” In reviewing the medical records, I came across a note saying that she was one of four family members living together who had all died of “fulminant sarcoidosis.” On AFB stain, her granulomata were full of Mycobacterium. That “fulminant” sarcoidosis was tuberculosis, and those family members didn’t need to have died.
Since they are small, a few granulomas here or there are no big deal, usually. If were all that bad, God would not have provided it as a defense for us to use. Everybody has a few floating around. If you’ve stuck a splinter in your finger, you probably have a microscopic bit of wood surrounded by macrophages. Or a bit of sand if you fell off a bicycle as a kid. Or walling off suture material if you’ve had surgery. But, as Hesiod noted in 700 BC, moderation is best in all things. Over time they can add up and start blocking things. In the lungs, that can result in pulmonary hypertension with resultant repiratory and cardiac complications. In the brain, they can block the circulation of cerebrospinal fluid or cause seizures or behavioral changes.
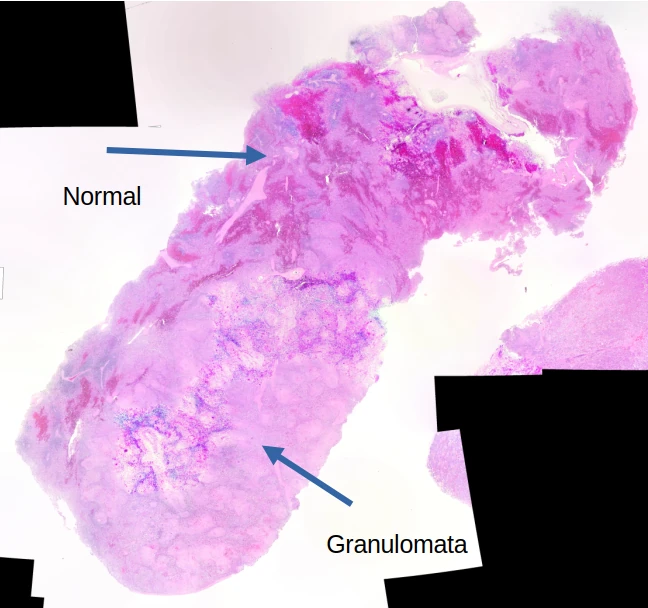
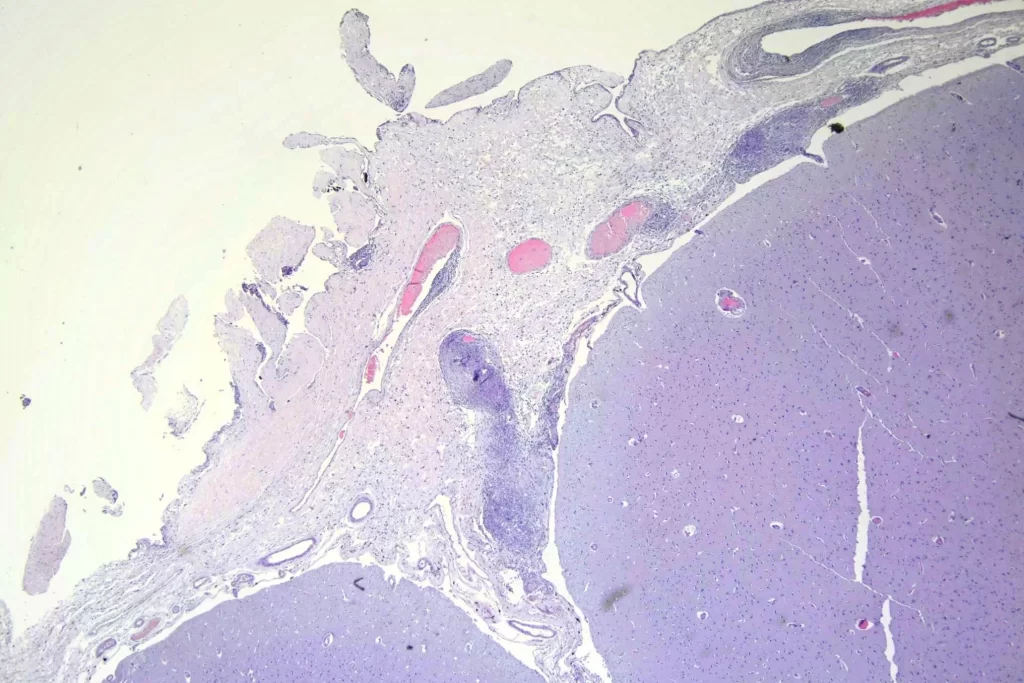
This first decedent had been diagnosed with neurosarcoidosis about a decade before his or her death, requiring a ventriculoperitoneal (VP) shunt. Autopsy confirmed the diagnosis of neurosarcoidosis, with additional granulomata noted in the lungs, liver, and spleen. On gross examination, the only real finding were large firm poorly demarcated nodules in the spleen. Here’s a gross photograph of a bit of spleen as well as severe right atrial dilation. Unfortunately, I didn’t think to take a photo of the spleen until after I’d dissected it, so it’s not the standard big section. You can see a sllightly ligher colored lump at the edge. That’s a whole bunch of granulomata that have fused together: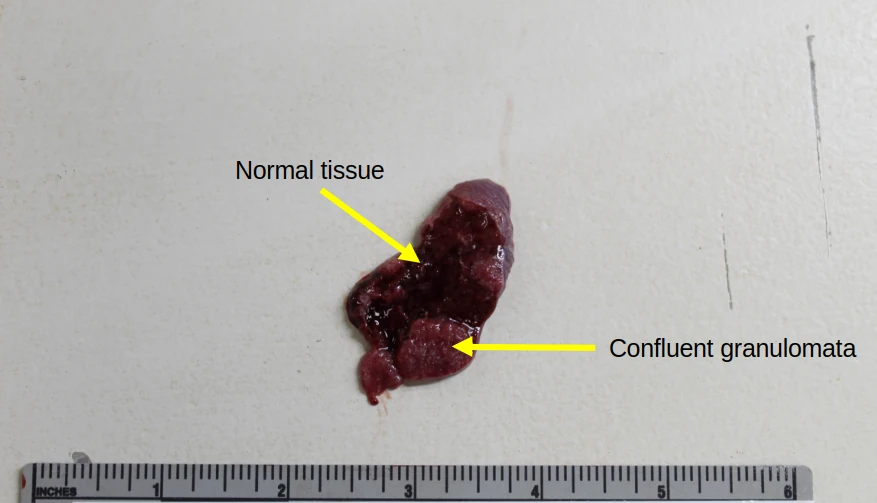
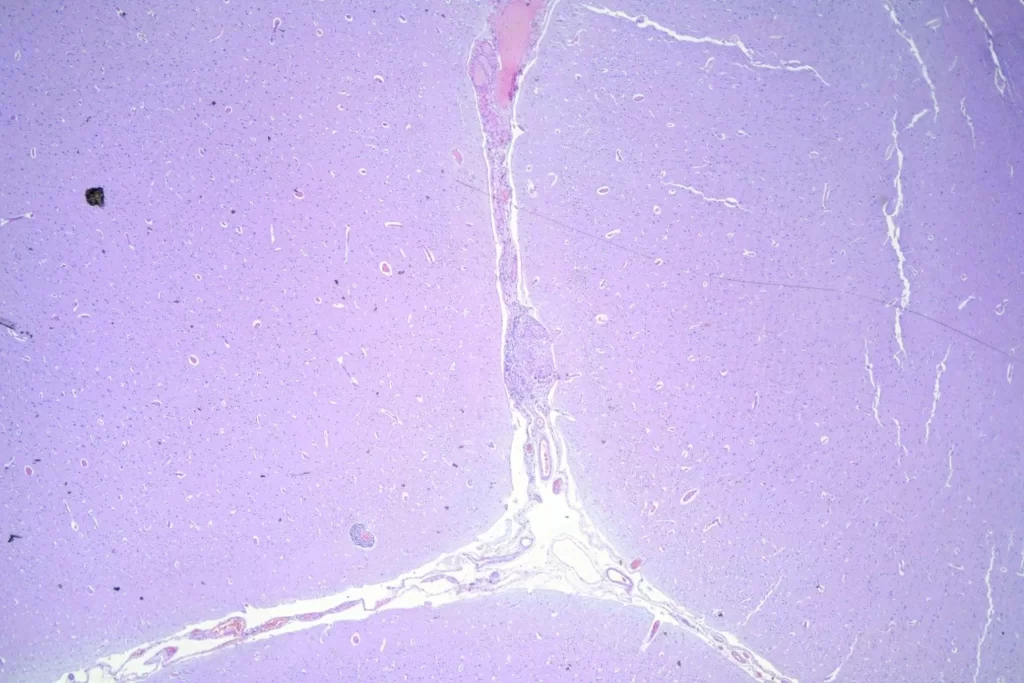
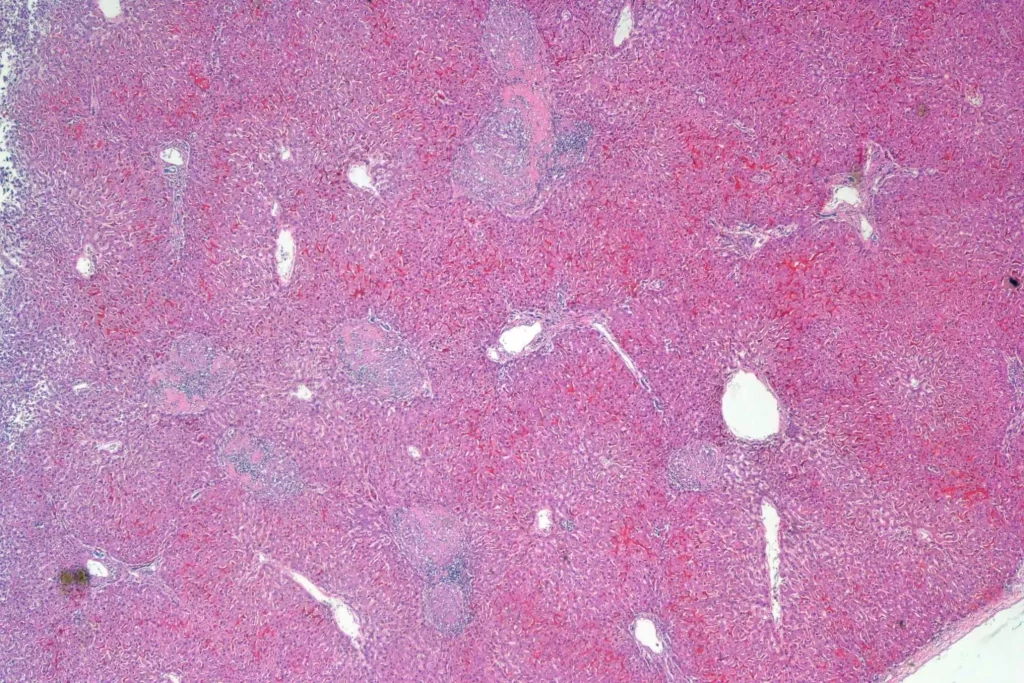
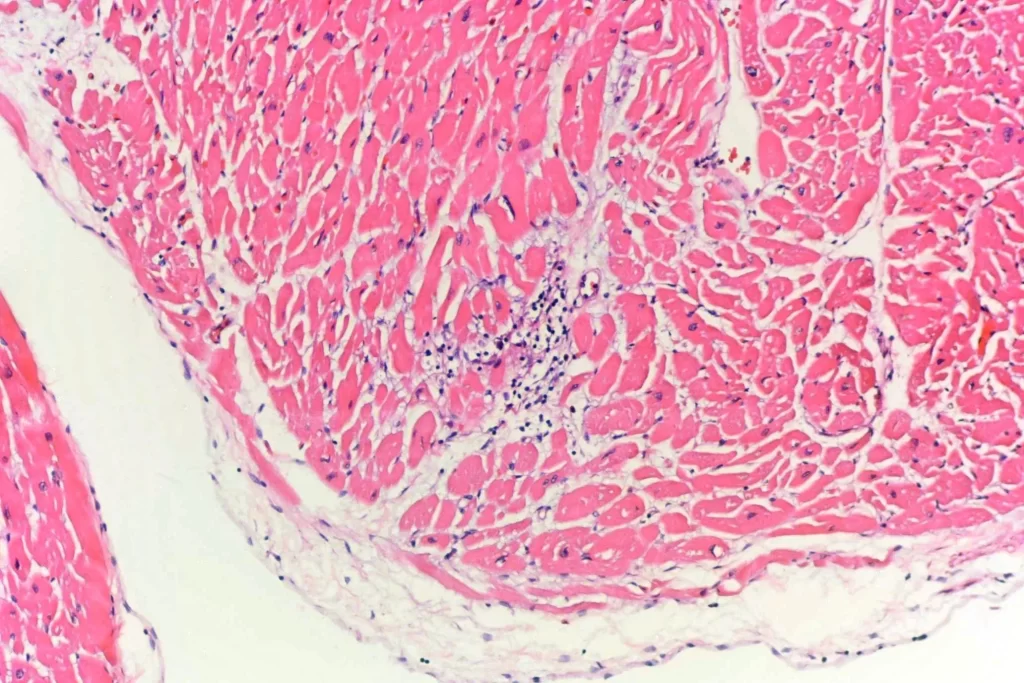
Here’s a panorama low power histologic view. Don’t look too closely — I had some problems with color balance putting the images together…
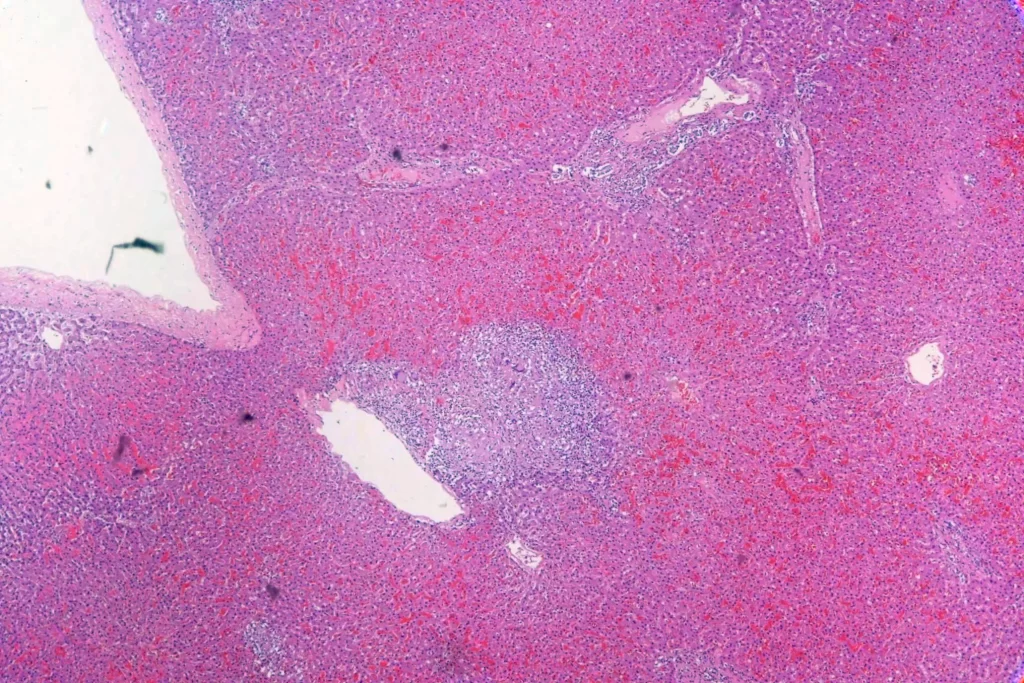
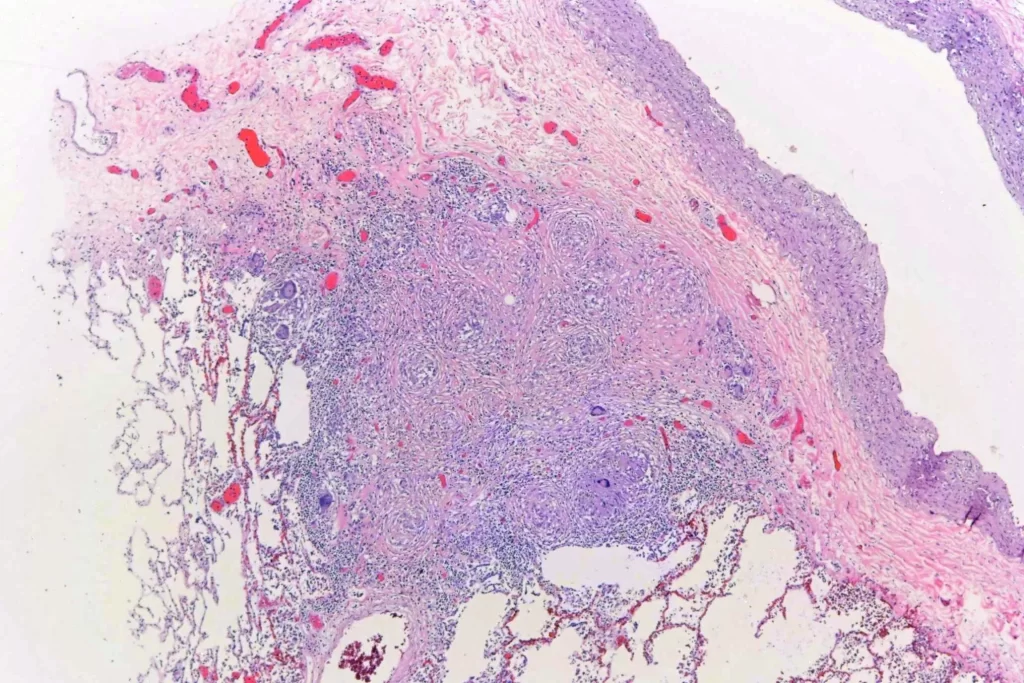
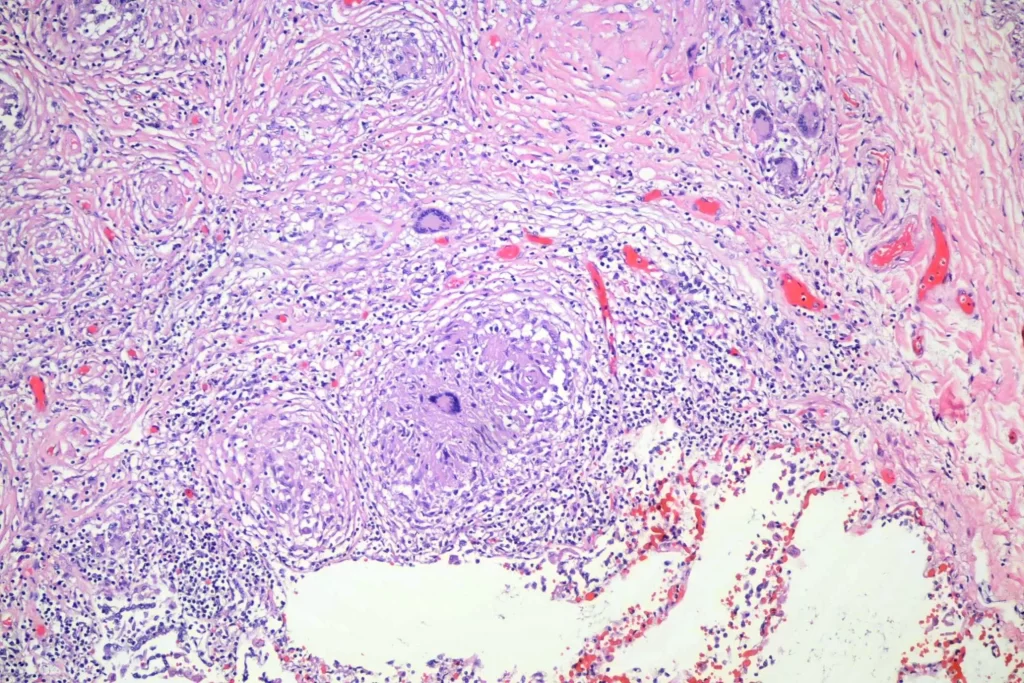
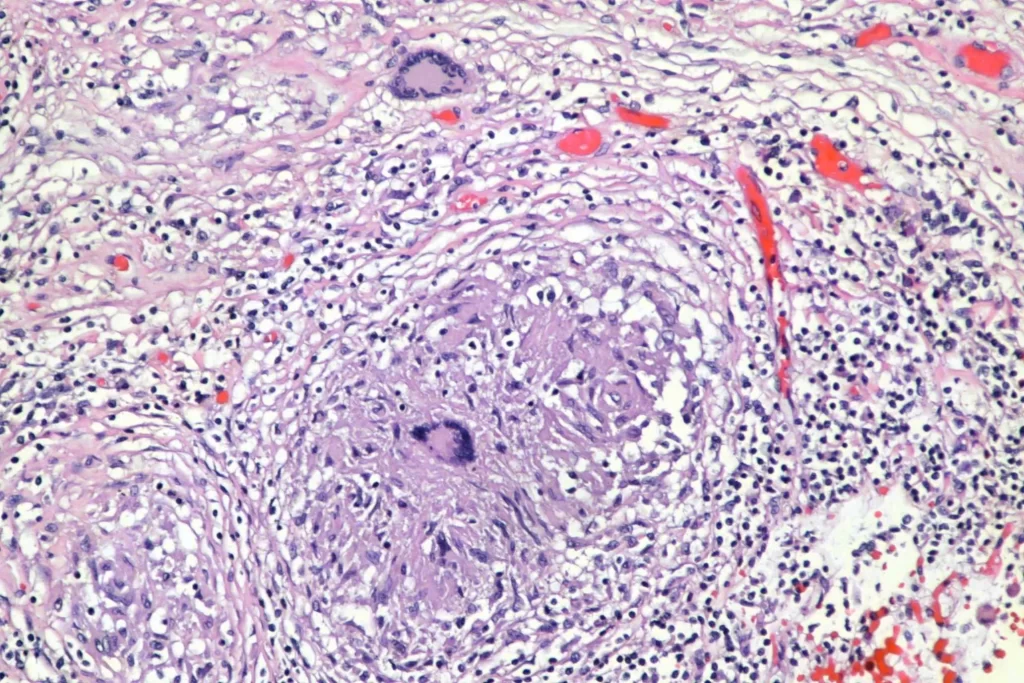
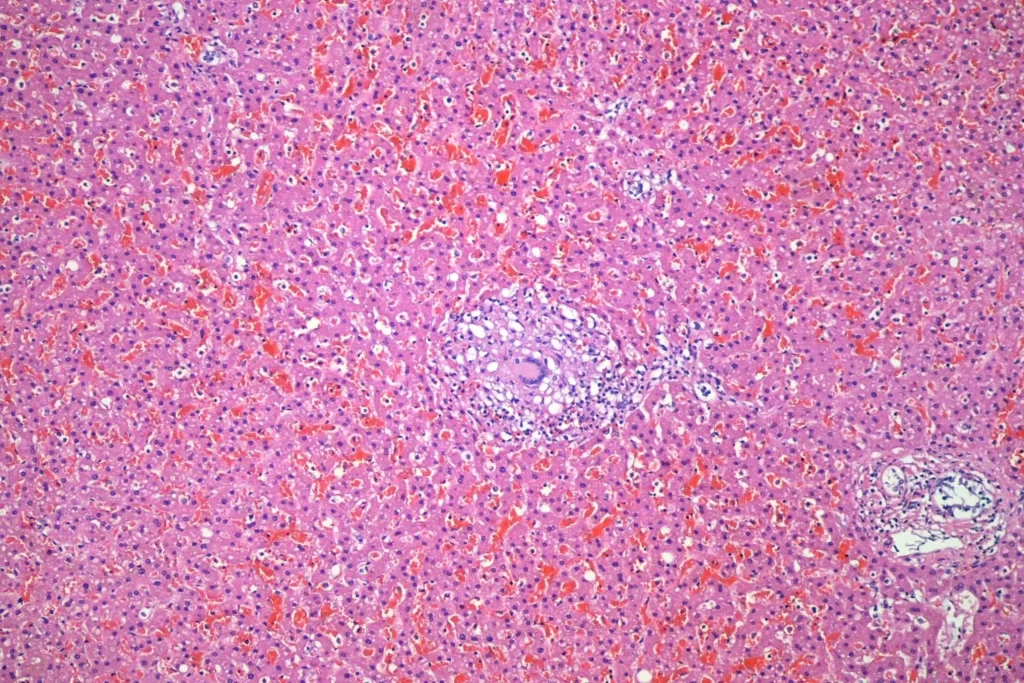
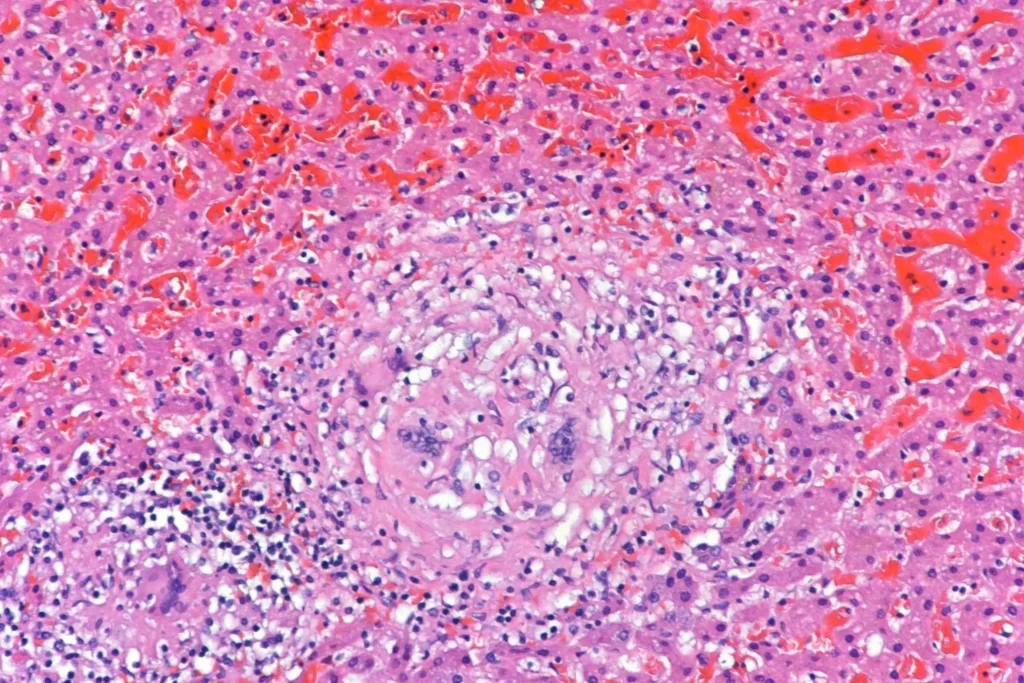
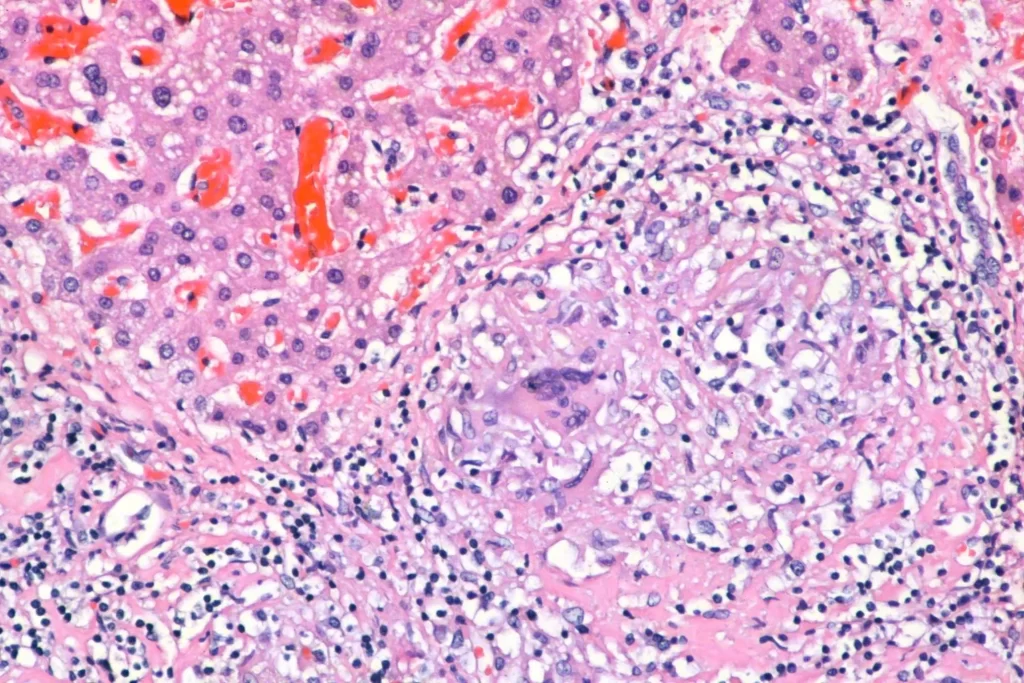
Here’s closer views of the splenic granulomata:
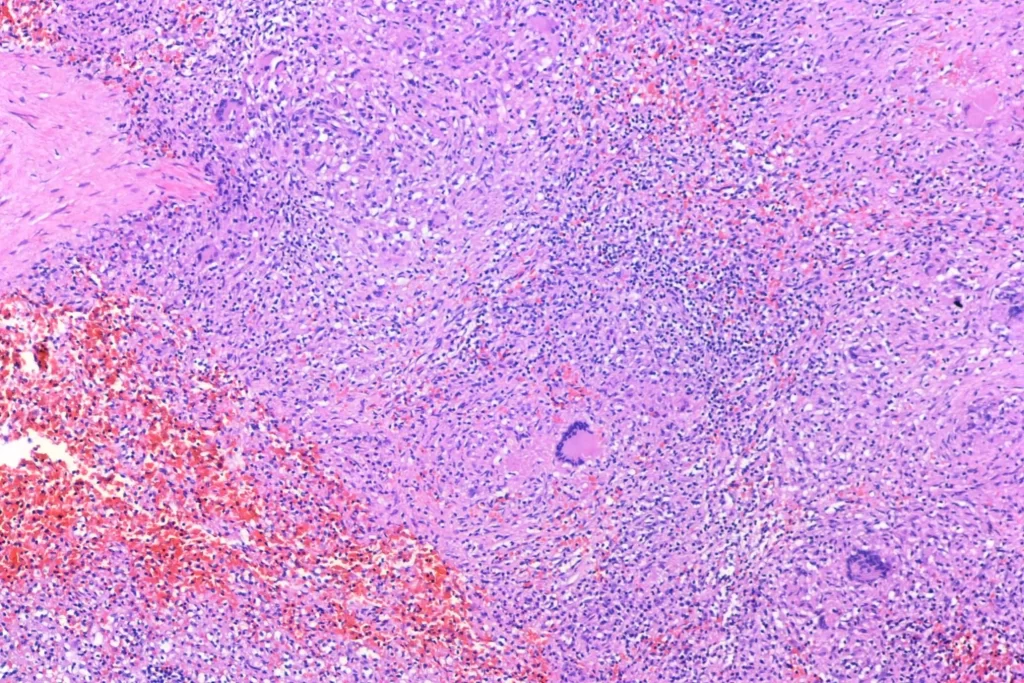
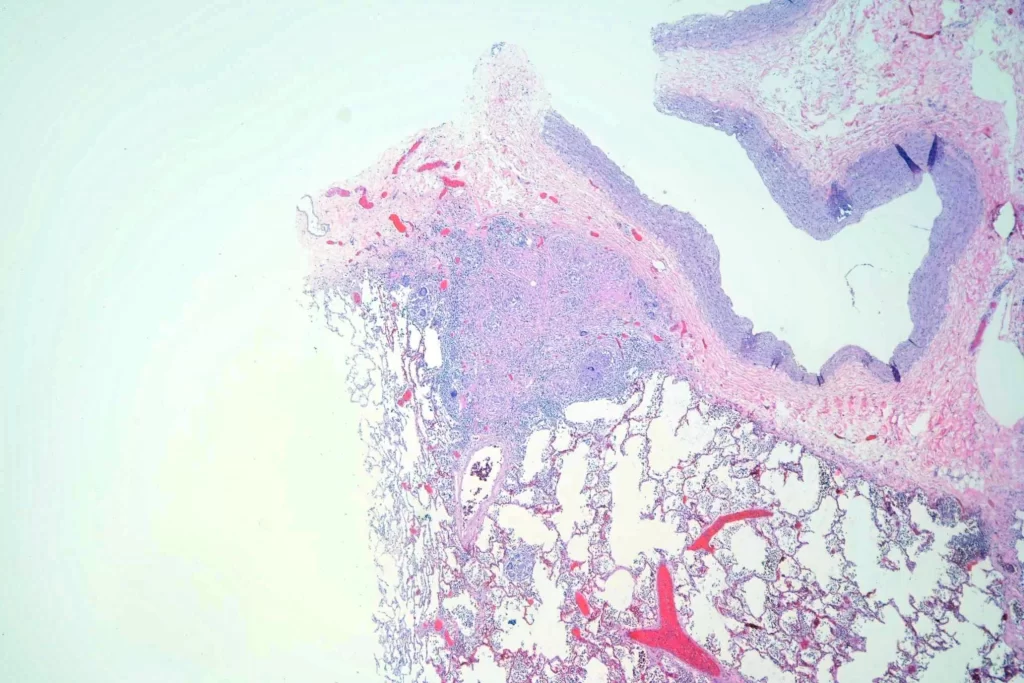
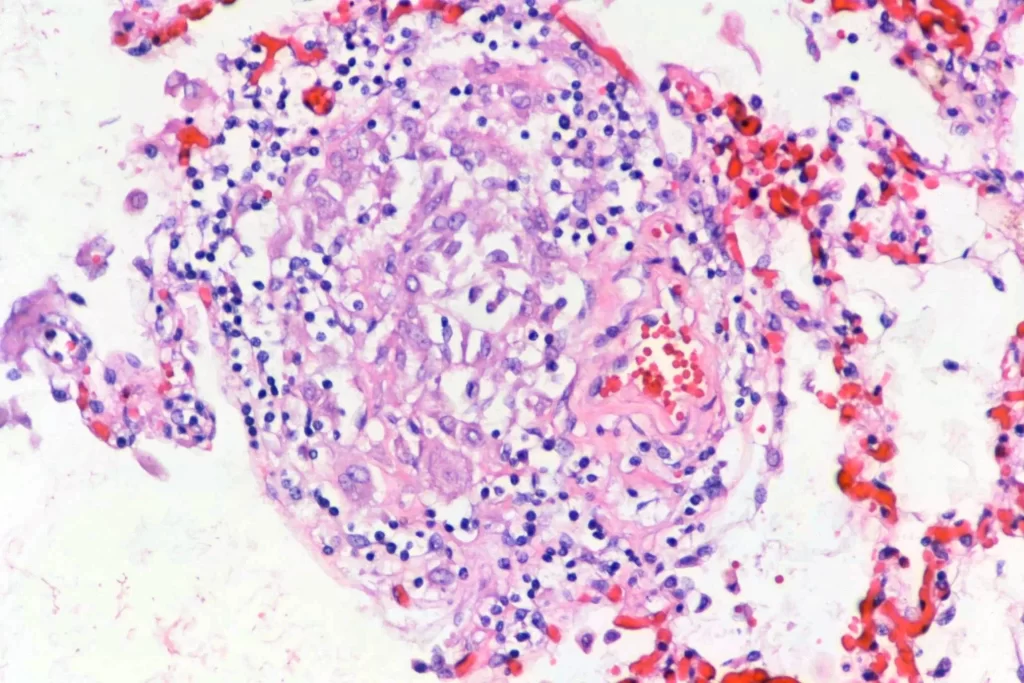
There were pulmonary granulomata:
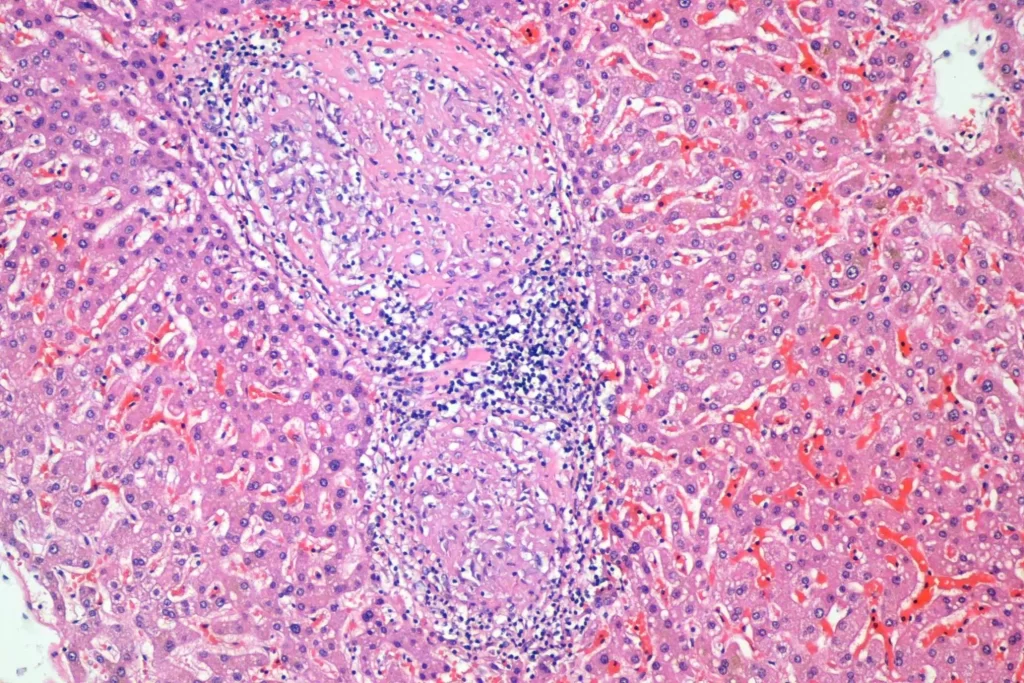
And granulomata in the liver:
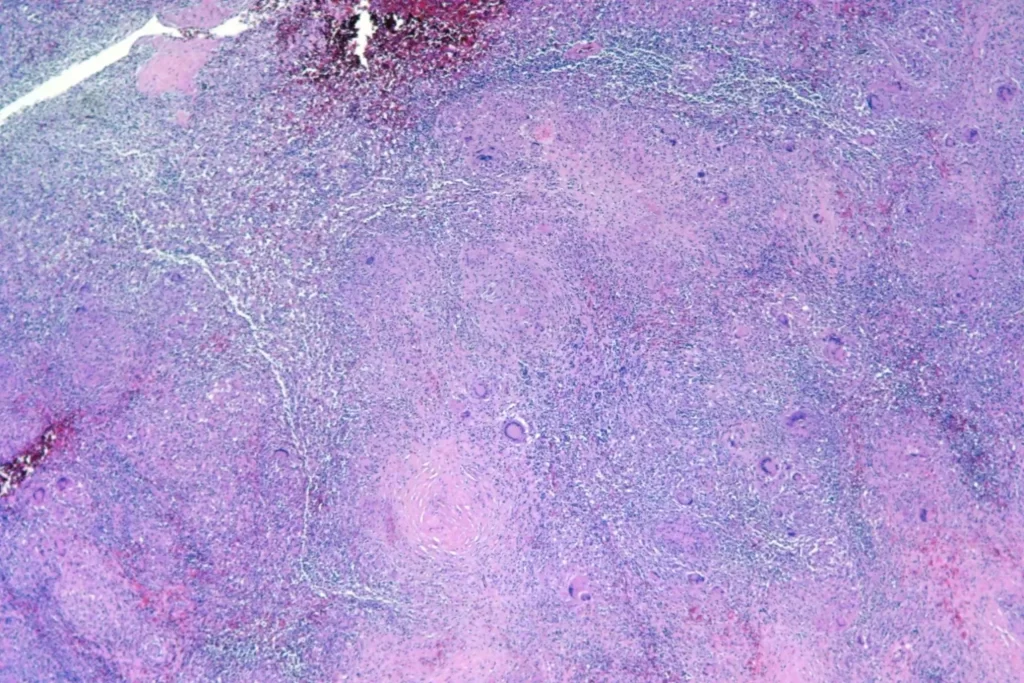
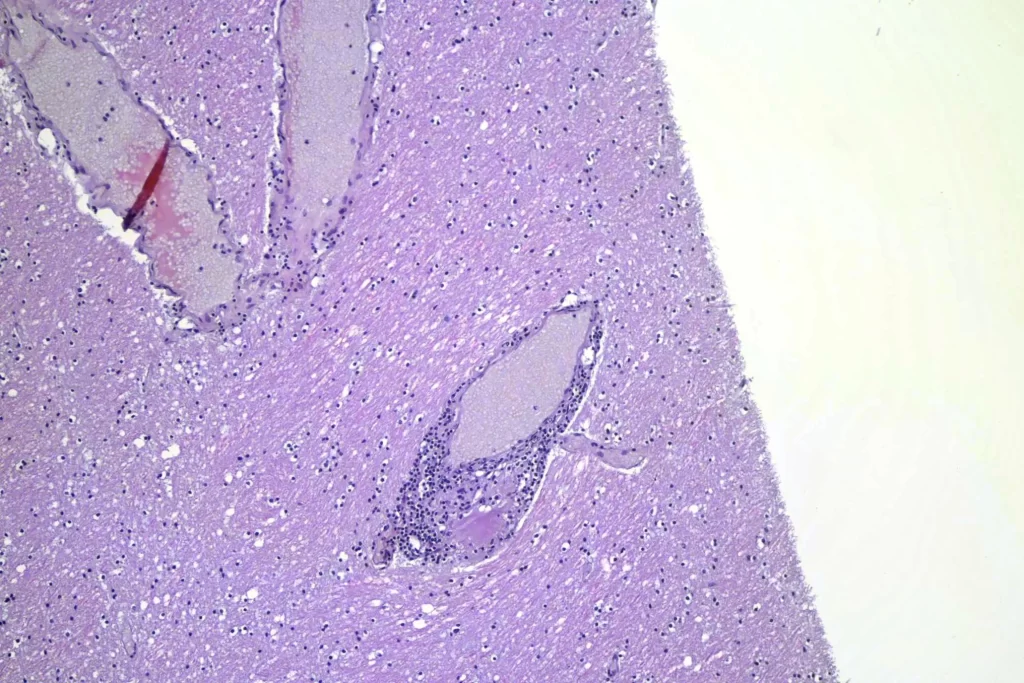
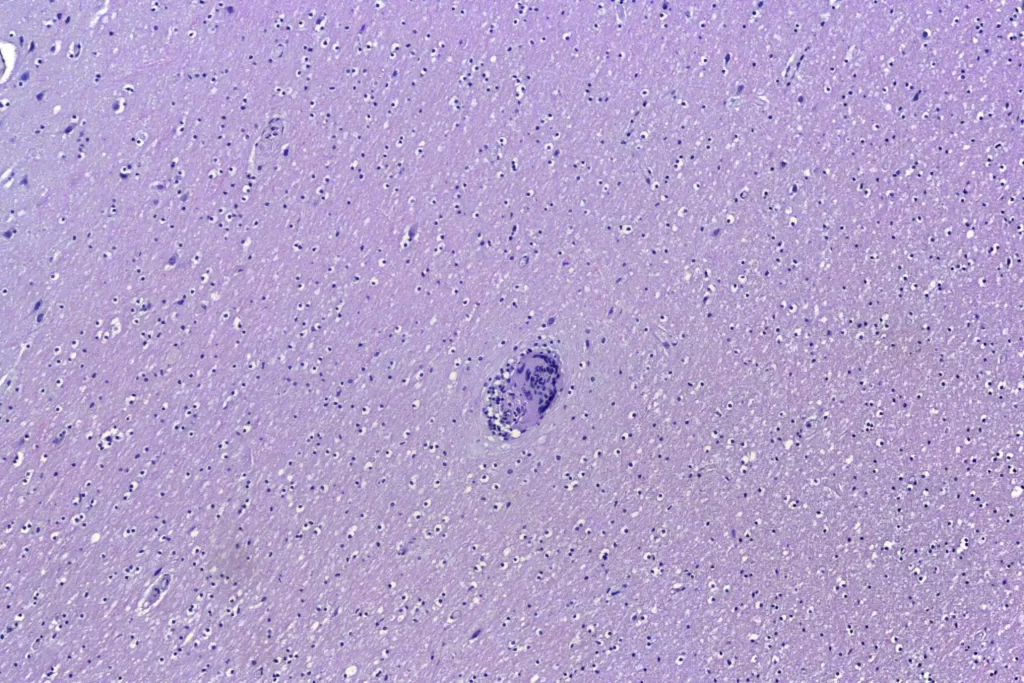
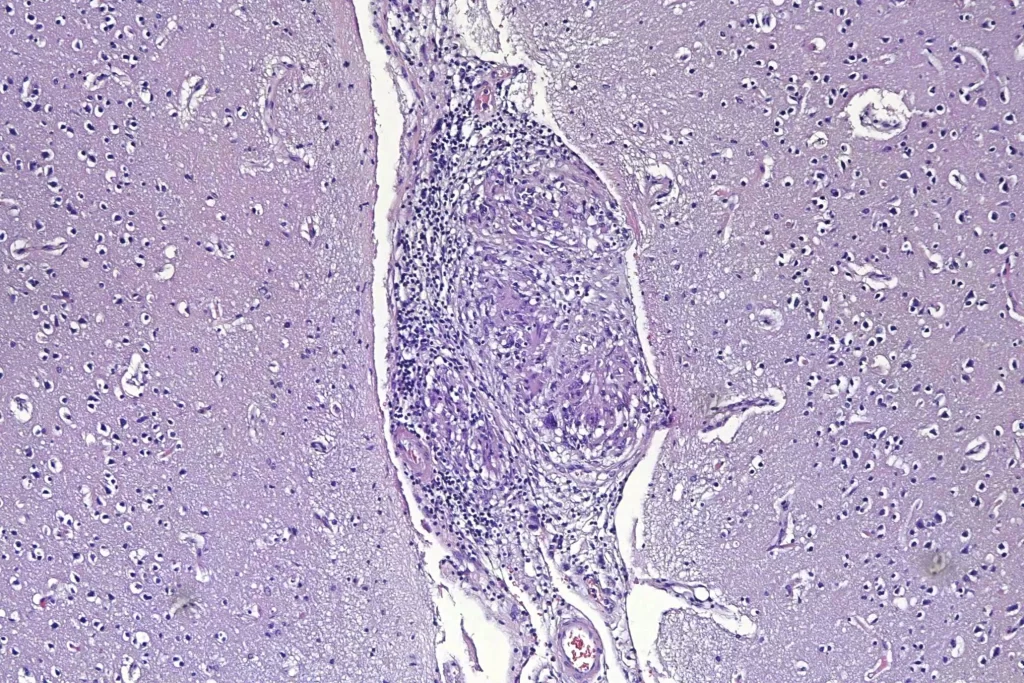
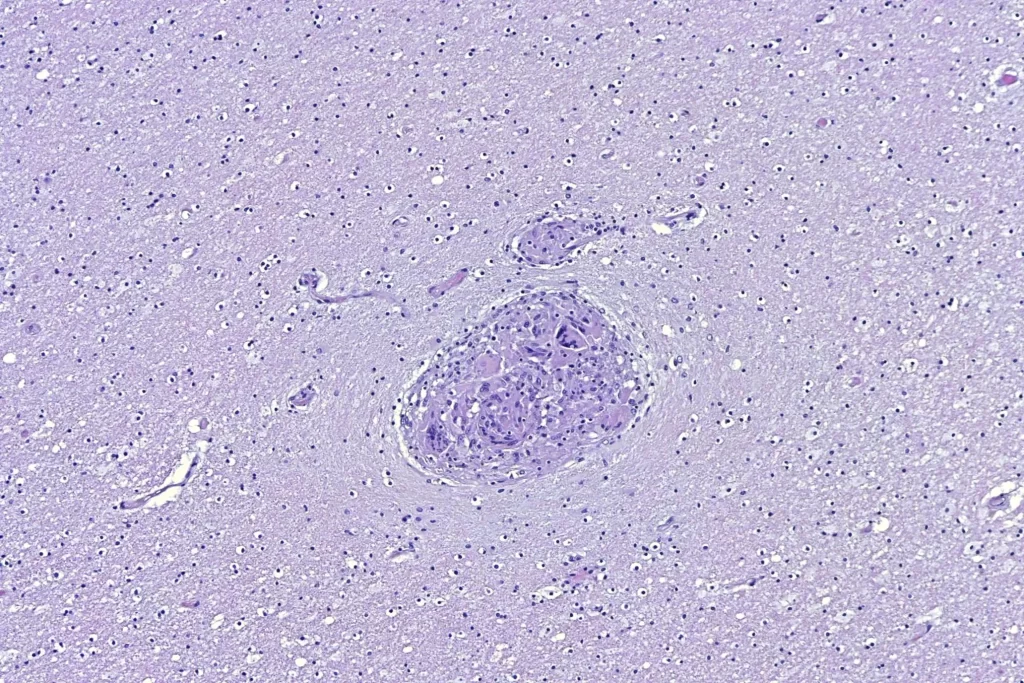
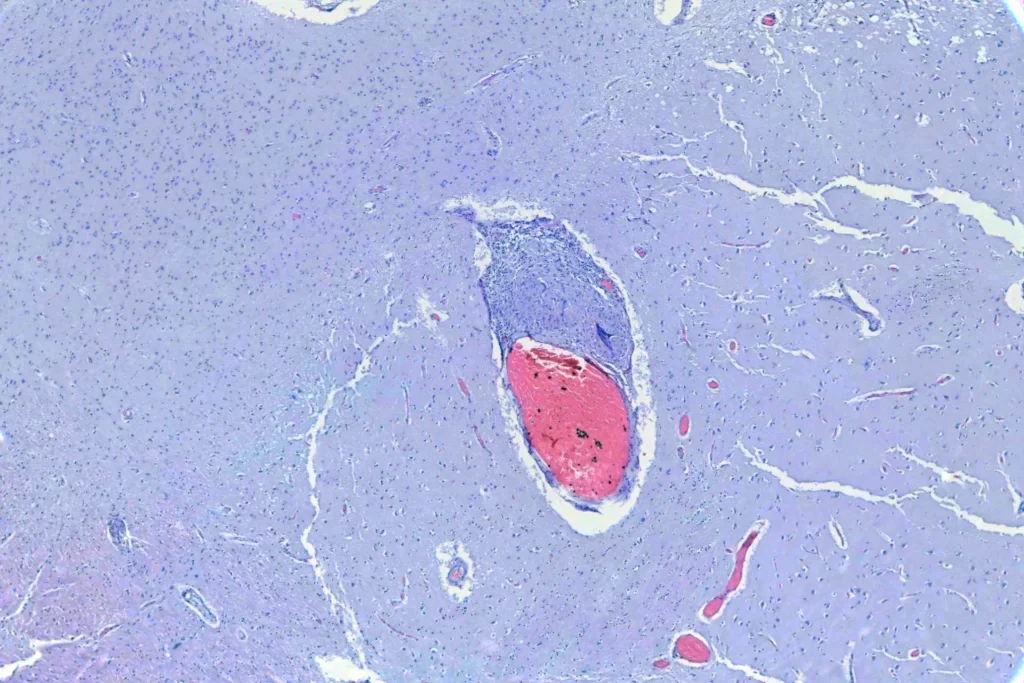
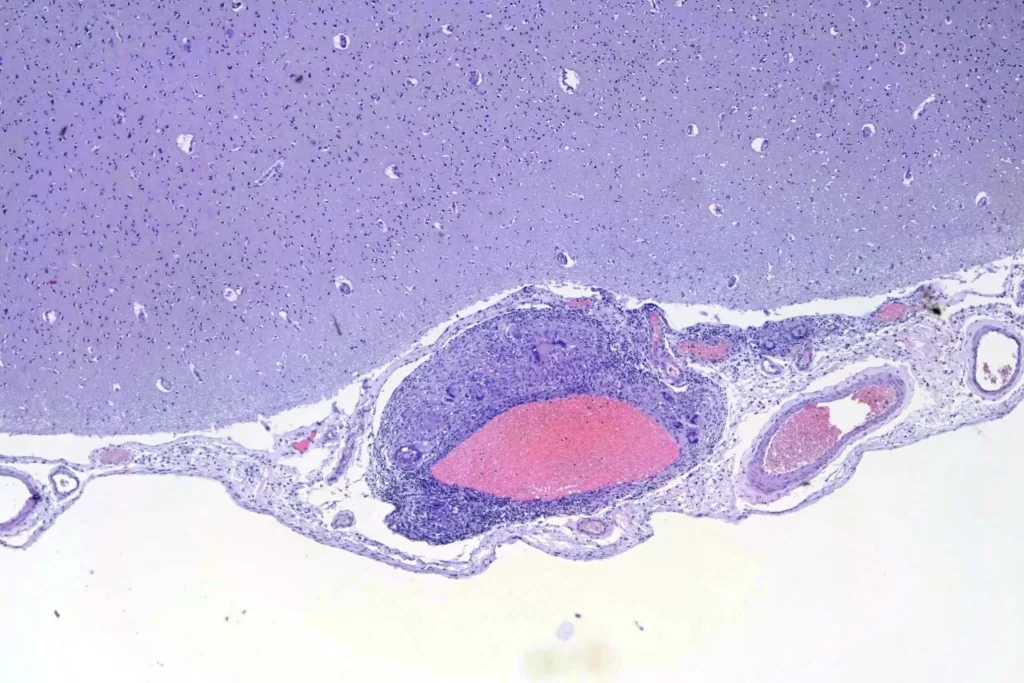
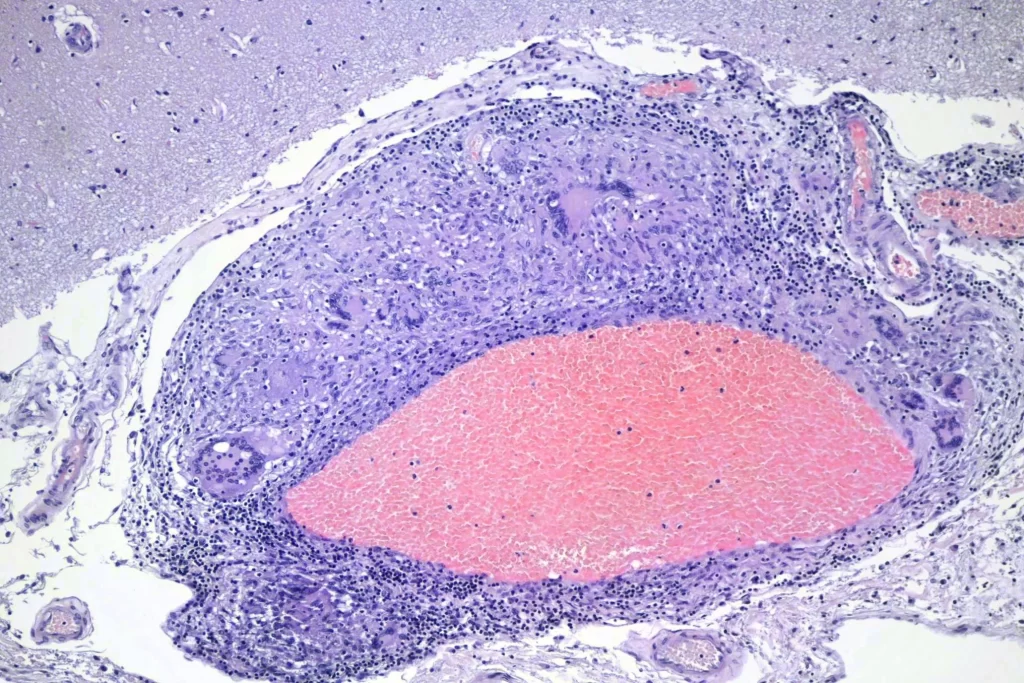
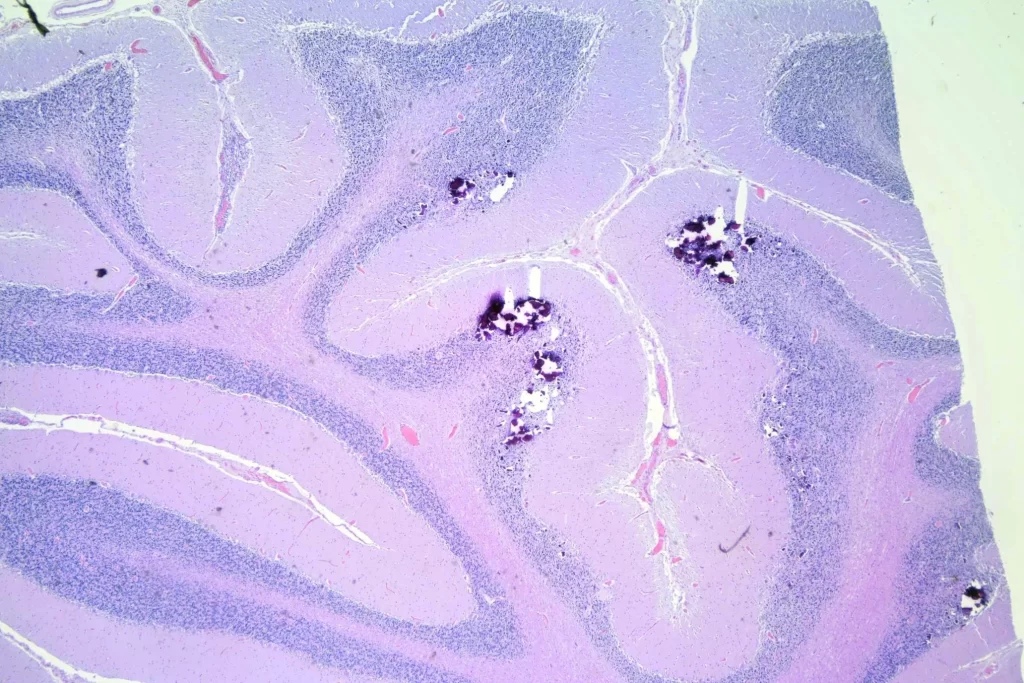
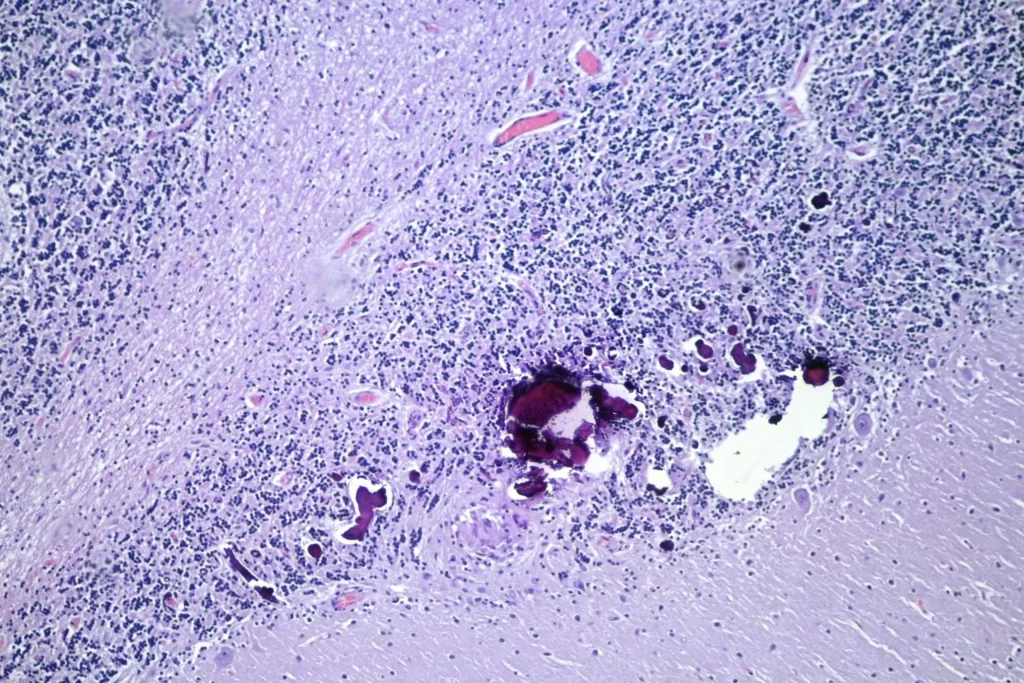
When I looked at the brain, granulomata were present in sections from all lobes, the cerebellum, the thalamus, and the brainstem. The granulomata in the parenchyma of the brain were smaller than those in the other organs. They were also common in the leptomeninges. Unlike the lesions in other organs, these were frequently perivascular. In addition, there was scattered dystrophic calcification in the cerebellum. Both the calcification and the perivascular distribution has been remarked upon in the literature.
And the calcifications:
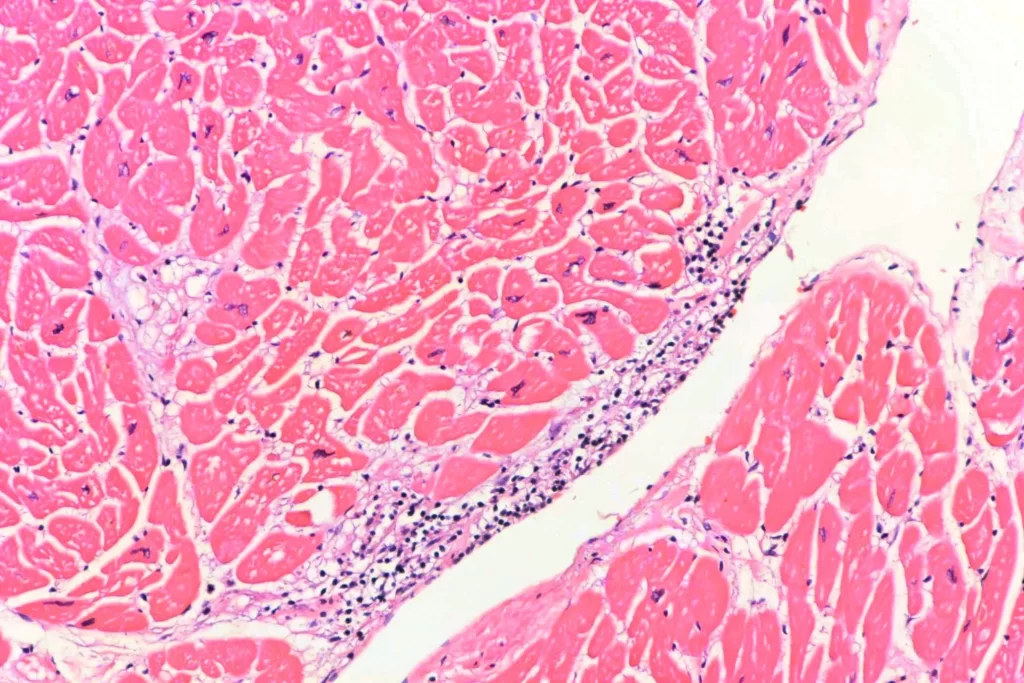
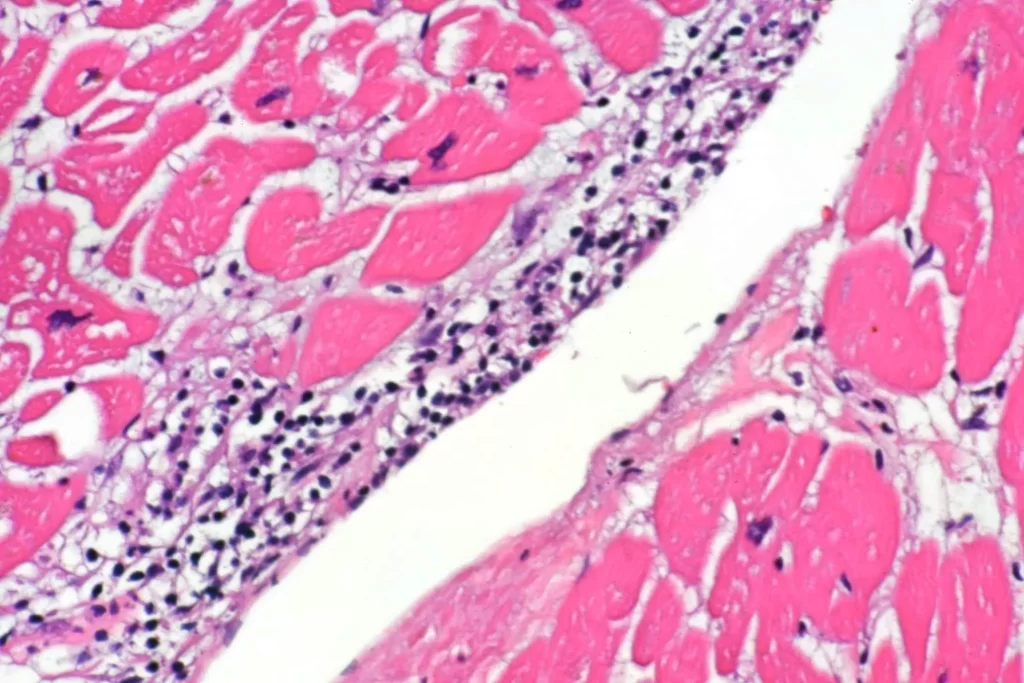
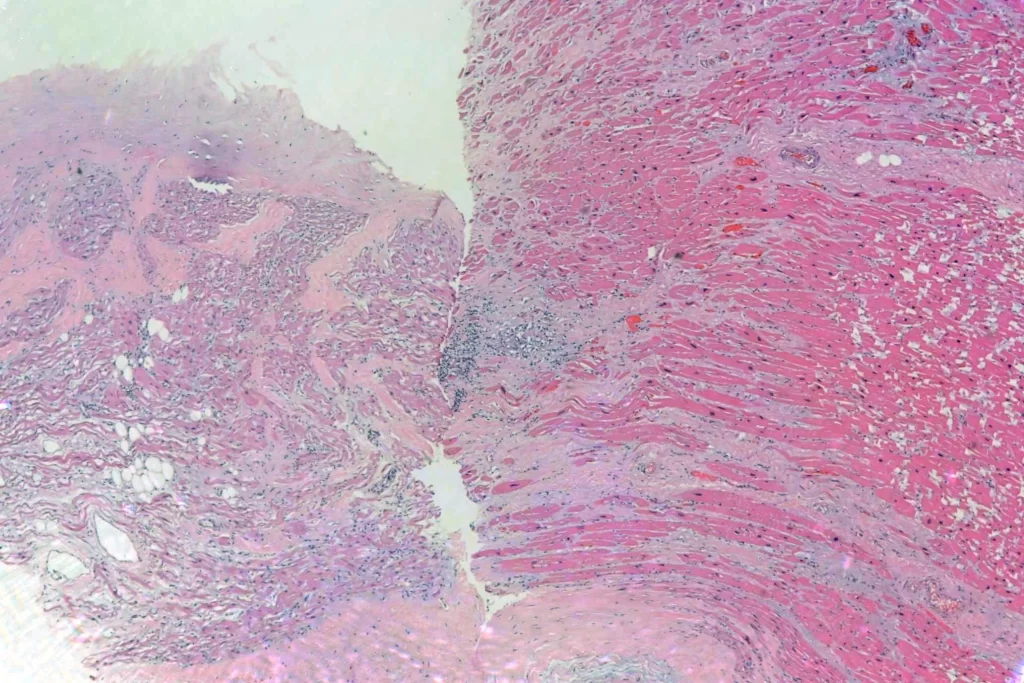
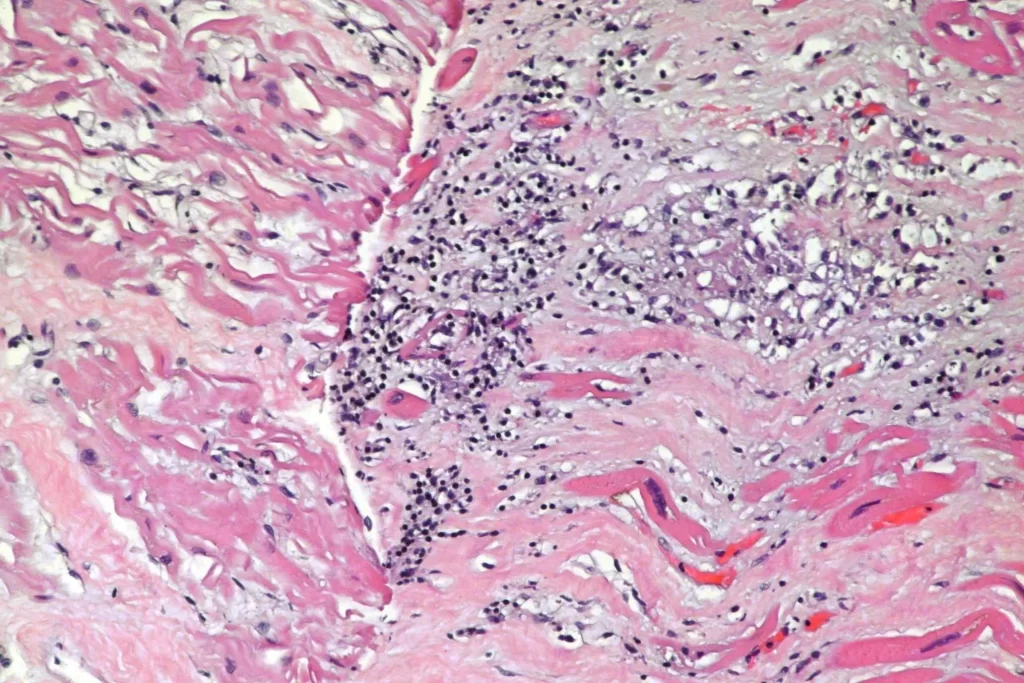
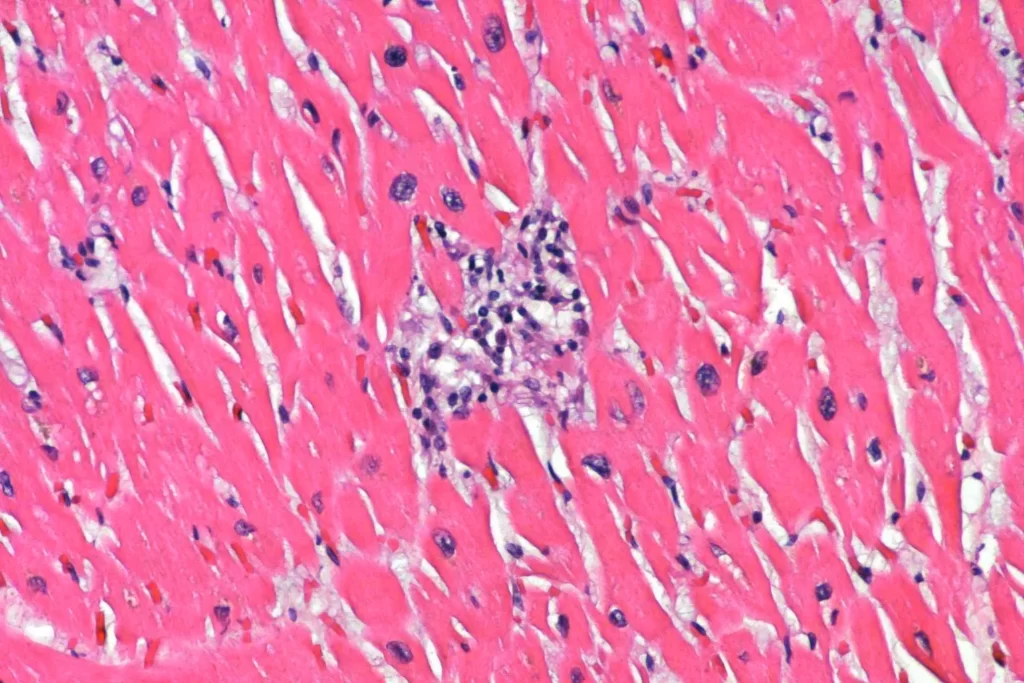
Finally, there was also a focal myocarditis without granulomatous inflammation. I don’t know if this was just inflammation that would eventually become a granuloma, or if it was a separate process. Methamphetamine can cause both infarction and myocarditis, so this might be an independent problem in this decedent. In the upper two photomicrographs, you see inflammation in the subendocardium. A couple of those cells that look a little like polymorphonuclear leukocytes in the photos are actually pyknotic myocytes when you can see them better in the scope. The second two photos are taken from near the atrioventricular septum (though the orientation is a bit unfortunate), which can be bad news.
The second decedent had not been diagnosed with sarcoidosis prior to death. The findings there are similar, though granulomata were present only in the liver and lung. Since this was not previously diagnosed, I went ahead and did GMS and AFB staining, which were negative. Since I had a cause of death already, I didn’t do further workup. Interestingly, the second decedent *also* had a teeny bit of acute myocarditis.
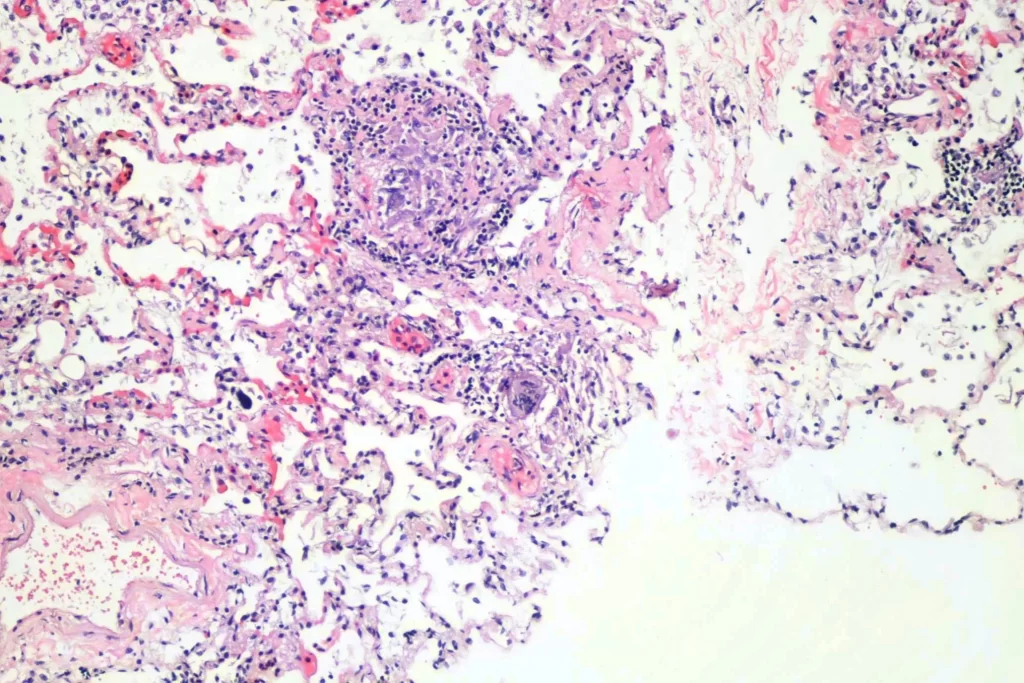
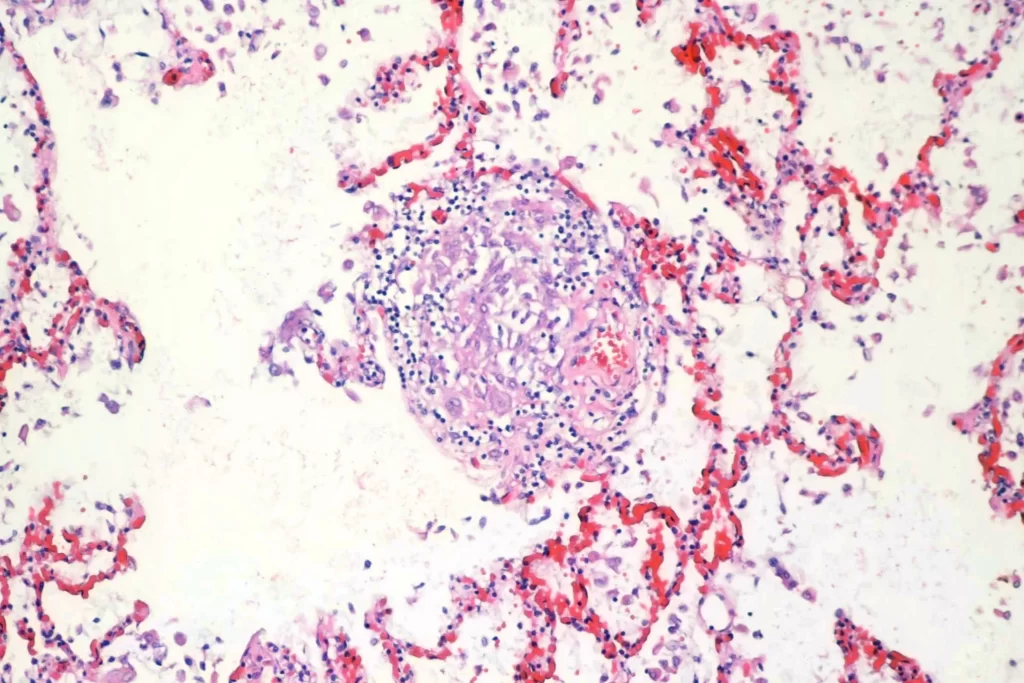
Here are some sections of the lung:
And liver:
And here’s the heart:
As always, free for use in lectures, etc. with or without attribution, though attribution is appreciated. If you need higher resolution images let me know.