A young adult male with a long history of poorly controlled type I diabetes mellitus died of diabetic ketoacidosis. The histology of his pancreas is characteristic of a victim of this disease.
First, it may be useful to review the structure of a normal pancreas. The normal pancreas consists of two large parts. The first is the “exocrine pancreas” that secretes digestive enzymes into the gut. The second is the “endocrine pancreas” that secretes numerous hormones into the blood, including insulin, proinsulin, amylin, C-peptide, somatostatin, pancreatic polypeptide (PP), and glucagon. The two that get the most press are insulin and glucagon, both of which regulate blood sugar. Insulin decreases blood sugar and glucagon raises it. The insulin-producing cells live as little balls or clumps of cells scattered in a sea of exocrine cells and are called “Islets of Langerhans.”
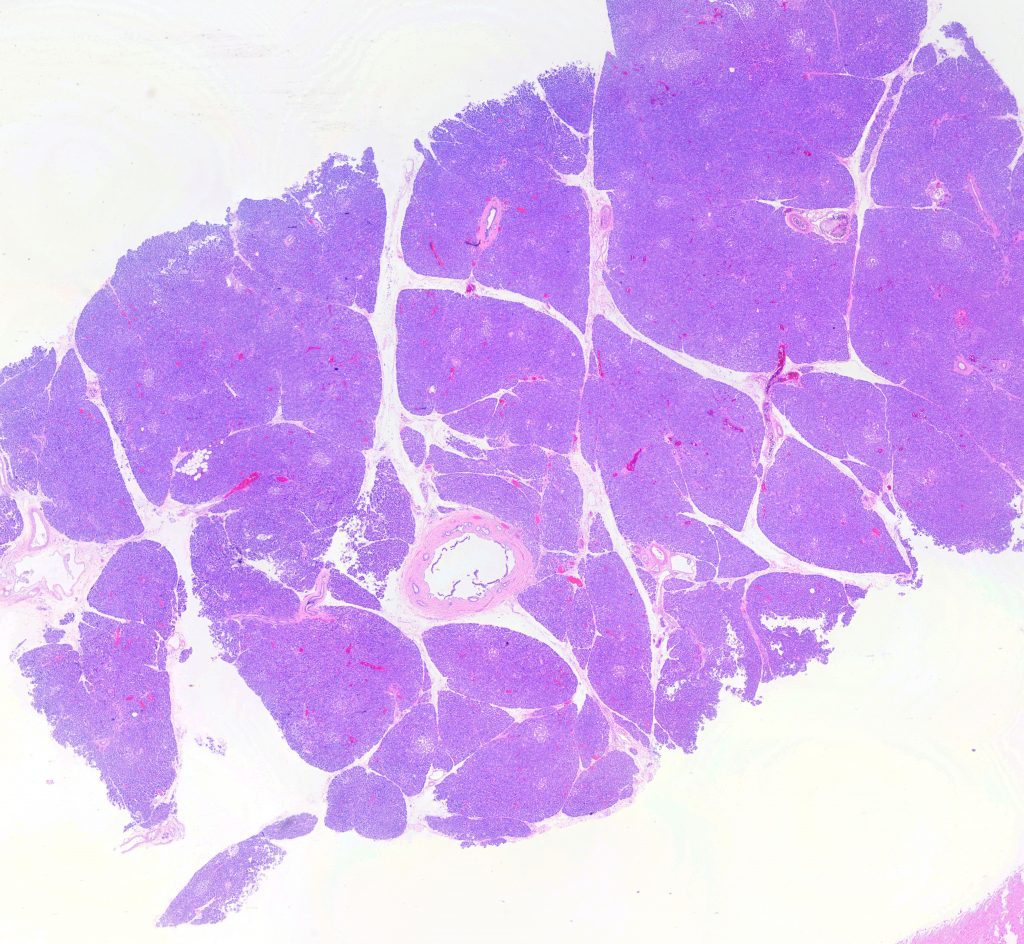
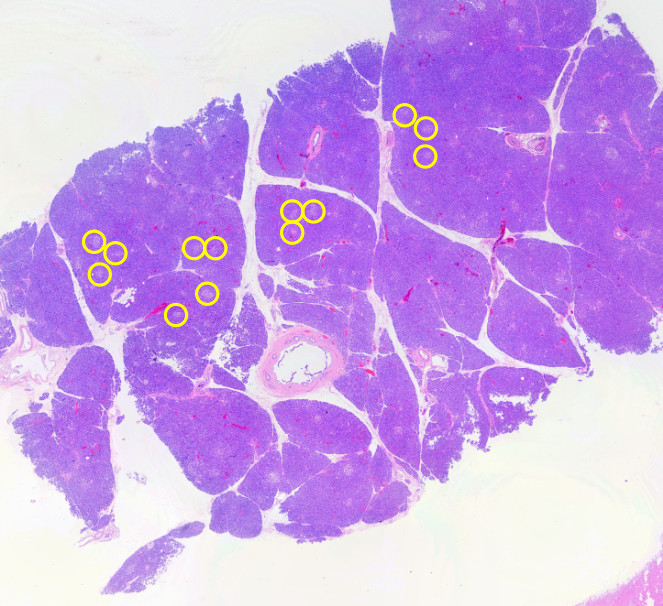
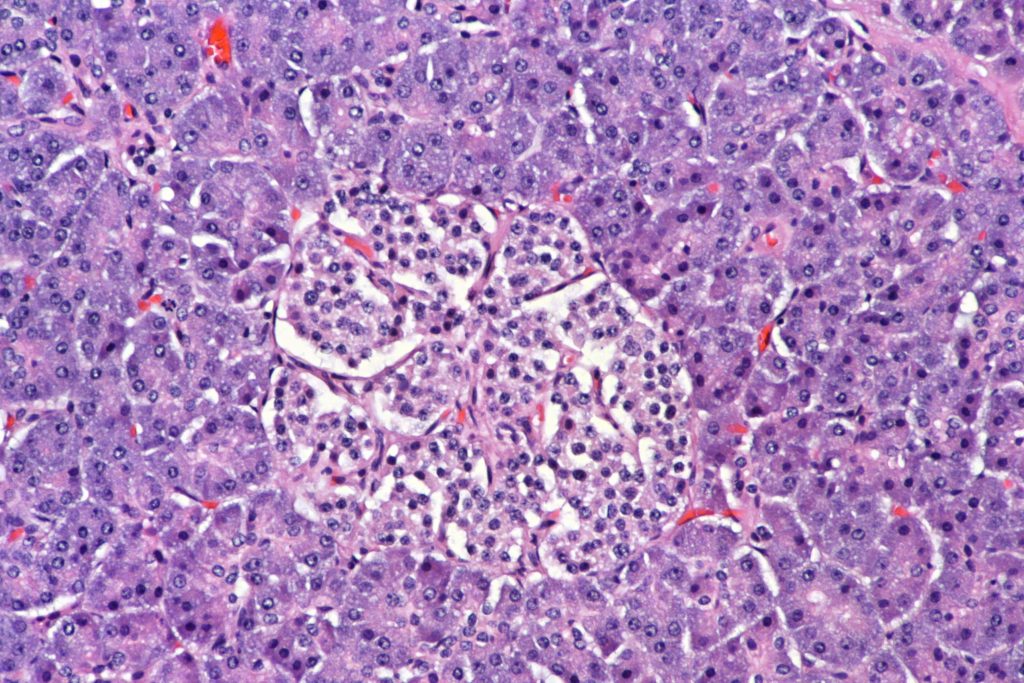
Here’s a picture of a relatively well-preserved normal pancreas. What you should be able to see is a relatively homogeneous blue background with small scattered light circles scattered about. The blue background is the exocrine pancreas, the small light circles are Islets of Langerhans. As always, double click or open the image in a new tab to see at higher resolution — where the islets are more obvious.
Here’s a few — by no means all — of the islets circled in yellow:
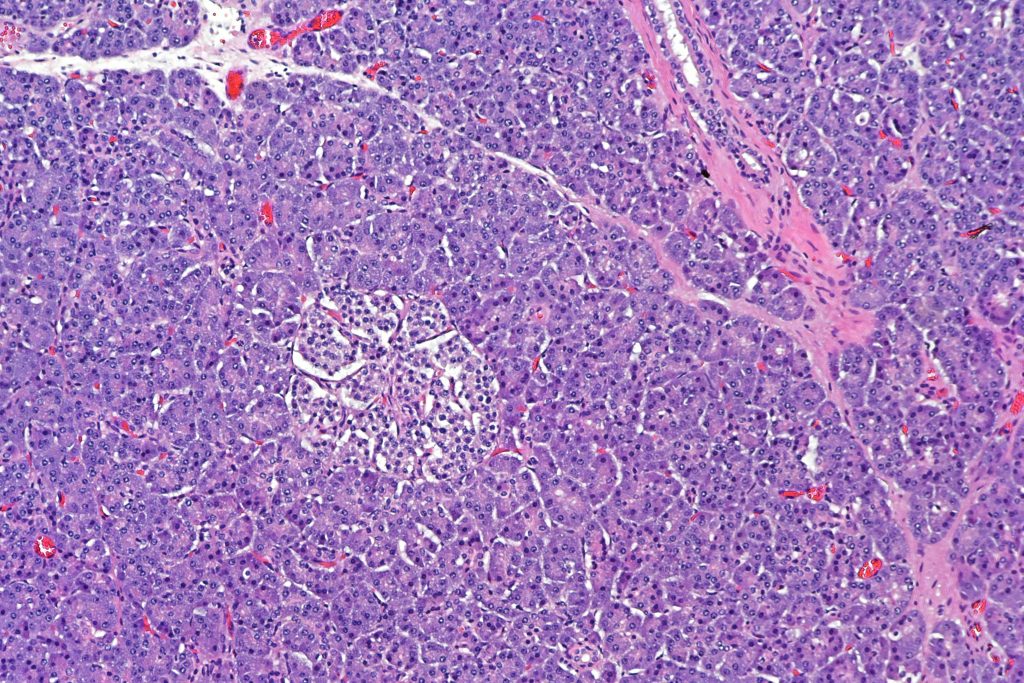
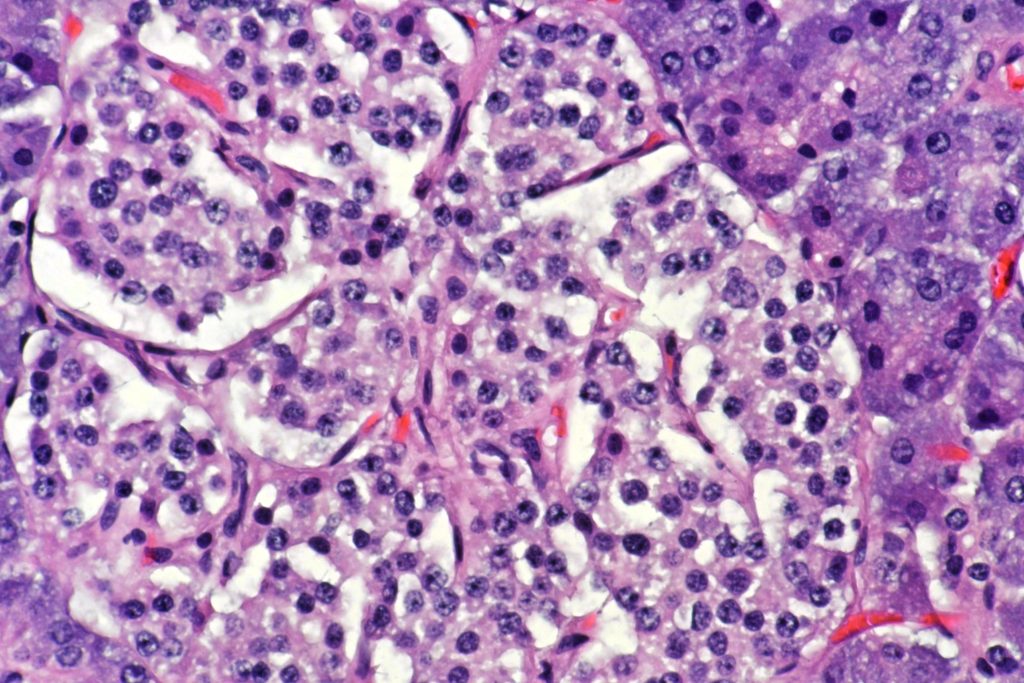
The darker cells of the exocrine pancreas are called “acinar cells” because they make up “acini” (plural of “acinus”). “Acinus” just means “sac.” You can see they are kind of oriented circularly around a center. The islet cells are more pale and seem a bit smaller. Here’s a higher power view:
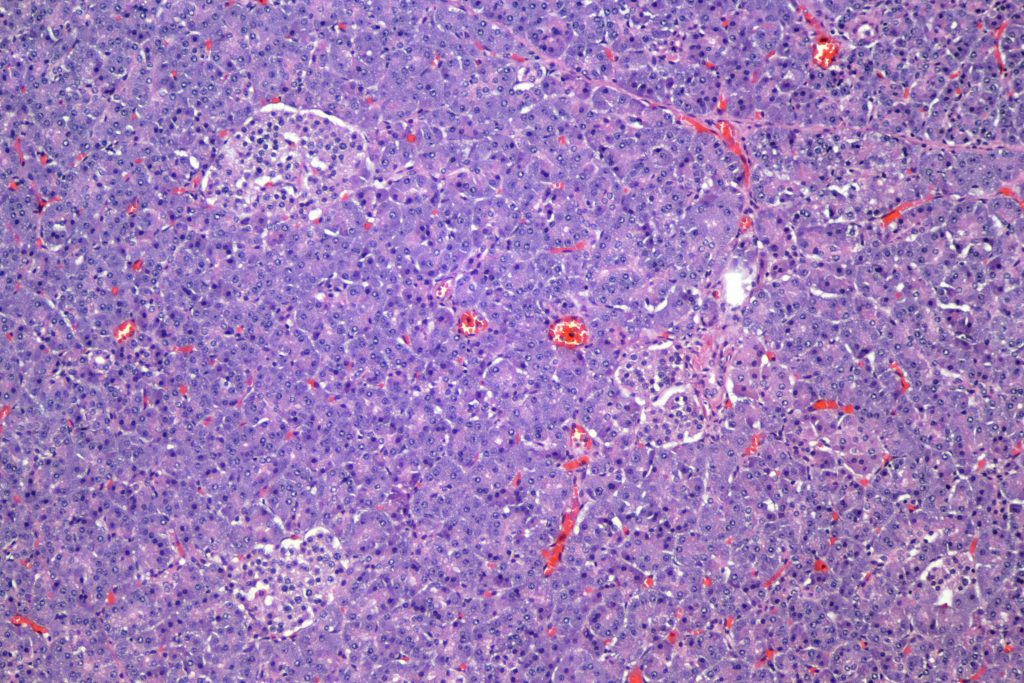
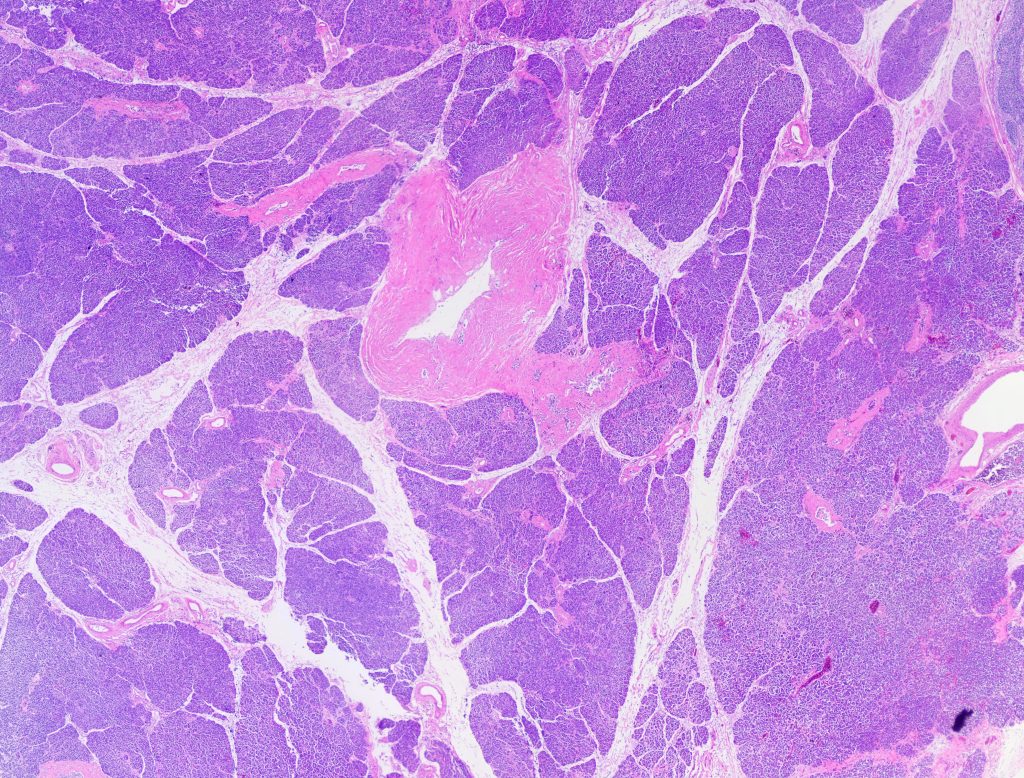
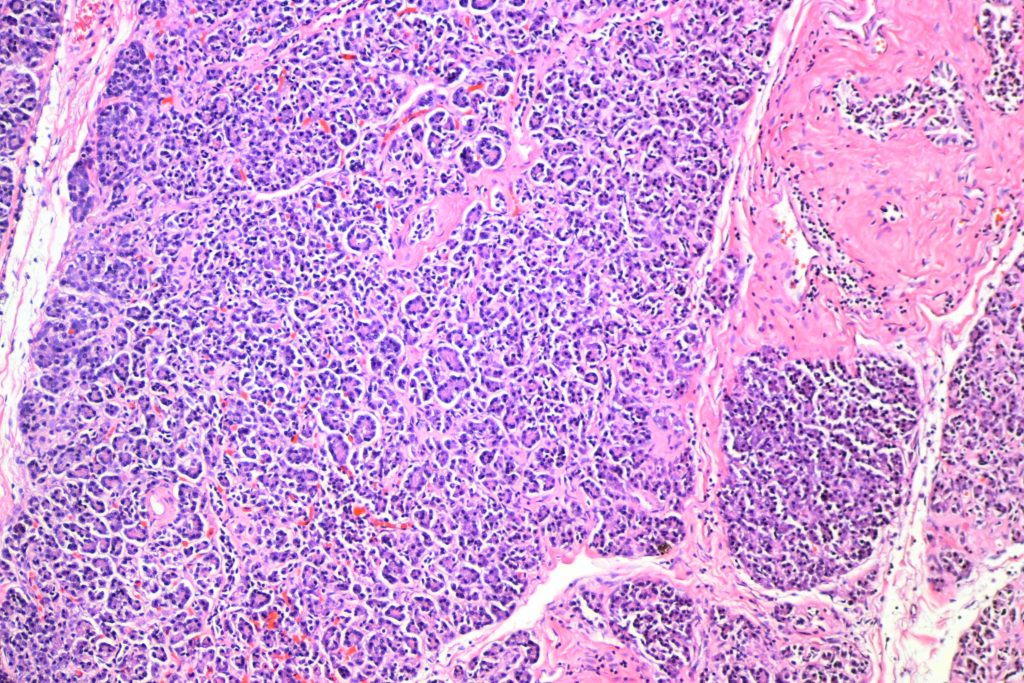
Now let’s look at the pancreas of a type I diabetic:
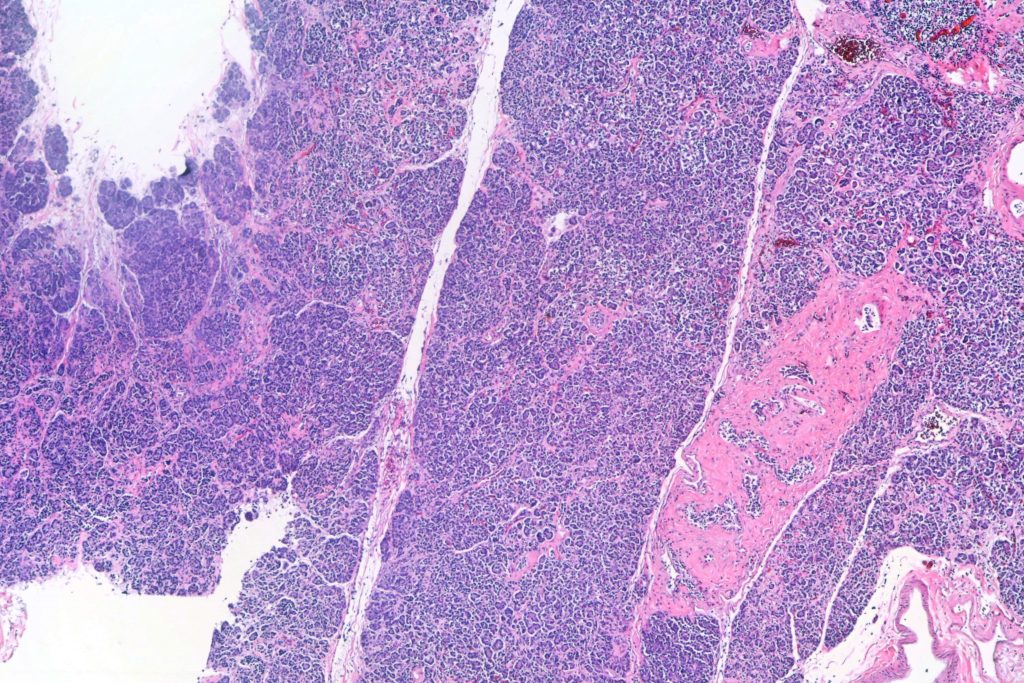
I hope you can see that there are no little light circles. Zip. Nada. None. It’s not a completely homogeneous blue, but that’s because there’s a little bit of fibrosis (scarring). Here are higher powers:
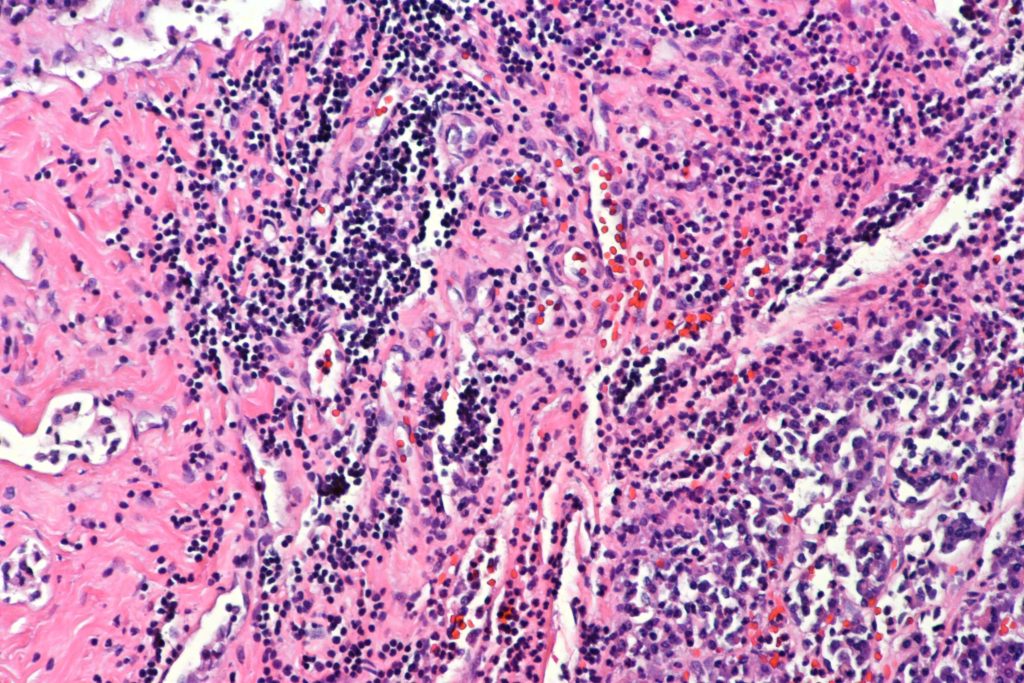
Note the increased fibrous tissue (pink), but no islets. Also, there’s a fair amount of chronic inflammation here and there:
People with type II diabetes are intermediate. They have a fair number of islets, but fewer than a normal pancreas. The islets tend to be smaller than normal islets, and have decreased insulin-producing cells and increased glucagon-producing cells. Interestingly, transplanting normal islets into immunodeficient mice will reverse diabetes, but an equivalent mass of islets from a type II diabetic will not (1). Special stains for inflammatory cells often reveal significantly increased inflammatory cells in the islets in this second type of diabetes.
As always, images are free to use for lectures and such. Attribution is appreciated, but not required. If you need a higher resolution image contact me.
- Deng, S., Vatamaniuk, M., Huang, X., Doliba, N., Lian, M.M., Frank, A., Velidedeoglu, E., Desai, N.M., Koeberlein, B., Wolf, B. and Barker, C.F., 2004. Structural and functional abnormalities in the islets isolated from type 2 diabetic subjects. Diabetes, 53(3), pp.624-632.