As I noted in the first post, a basic concept in cause of death determination is an understanding of the interplay between vulnerability and insult in the cause and mechanism of death. I touched on it before, but I’m going to go into a little more depth here. It is part and parcel of every case we do. Sometimes the understanding is implicit or even theoretical, and sometimes it it is explicit.
Here’s an example of the former. Every year, a number of infants die suddenly at home. Back when I was first in training, these were classified as “SIDS” (Sudden Infant Death Syndrome). Nobody really knew why these infants were dying — they tended to have either cold normal autopsy results or minor nonspecific findings. Then, folk started to see correlations between sleeping conditions and death, and a consensus started to grow that a significant number of these were asphyxial deaths. Animal studies showed that dogs placed in a condition where their heads were placed near bedding would rebreathe exhaled air and slowly suffer from oxygen deprivation and increased carbon dioxide concentrations. Other studies supported this. This in turn lead to the “Back to Sleep” campaign, which was correlated with a decrease in these deaths. Now there is a consensus that “unsafe sleep” conditions contribute to many deaths. The determination of the absolute danger of any particular sleeping arrangement is a matter of dispute, and my personal opinion is that the pendulum has swung a little bit too far in the direction of calling everything dangerous, but it’s clear that there is a line somewhere where the risk is significant.
But here’s the thing. Most kids do fine regardless. Mothers have been sleeping with kids in their arms since we were living in caves. And they don’t die. Mostly.
But sometimes they do die. Why? One common thought is that the kids who die and are not the victims of an overt overlay event have some small developmental delay or anatomic variant that makes them just a little more susceptible to small positional challenge to the ability to breathe. The arousal system that makes them wake up and move their head out of danger is just not quite developed enough — though it will be in another few weeks or so. Or their ability to clear fluids out of their airways isn’t quite far enough along. Or they have a genetic variant in their heart that makes them just a little more susceptible to lowered oxygen saturation in sleep. Or something. But the bottom line is that they have this one small vulnerability that most kids don’t have, and if you match that one vulnerability with just the right physical situation, the child dies.
When these deaths are classified, a few people still call them SIDS. Most, however, do not. Most folk now classify the deaths as “Asphyxia” due to “Unsafe sleeping conditions” or something like that. Do we add the vulnerability? Usually not, for two reasons. First, and foremost, we don’t really know in any individual circumstance what it is. The second is that because this is a convention, the vulnerability is part of the definition — it is a tautology. It’s unfortunate, because some prosecutors now want to prosecute parents for abuse because they should have known the danger to their child. But it’s not that simple, since the vast majority of kids do fine. You just don’t know if *your* kid is the exception to the rule.
An example of the latter might be a pulmonary embolism. Let’s say a middle-aged woman suddenly complains of shortness of breath and dies. At autopsy, she has a large pulmonary thromboembolism. On exploration of her legs, she has a large clot behind her left knee. The cause of death is “Pulmonary thromboembolism.” There is no real way to know where she got that original clot in her leg — it is likely weeks or months old. And there’s no way to know exactly what caused the fragment that killed her to break off right when it did. Often these occur when people are inactive for some time (which encourages the clot to form and/or grow) and then become active (which encourages a fragment to break off).
Sometimes that history is clear. A man breaks his leg and is in a cast for two months. He gets his cast off and immediately goes to the gym and starts doing leg exercises, becomes short of breath and dies. When I was in medical school I had a case of a college football player who suffered moderate trauma the previous season and was laid up for awhile. Then, the next year, every time he went to football practice he became short of breath. He was breaking of bits of clot from his pelvic veins when he scrimmaged.
But most of the time you don’t actually know. What you do know in a lot of these cases are risk factors — obesity, hormone therapy, diabetes mellitus, tobacco use, hypertension, etc. In these cases, it is thus common to add these risk factors as “contributing factors” or “Other significant conditions” on the death certificate. Had the decedent been a little less obese, or had not been taking oral contraceptives, or whatever, they *might* have not developed that clot. Though, really, you don’t know for certain. Still, you can’t ignore it — because it’s important to have those risk factors on the death certificate for public health statistics. Not every smoker who gets lung cancer got it “because” they smoked. But it’s important to keep track of that kind of thing, and in general it *does* contribute to the development of lung cancer.
As forensic pathologists, we are mostly concerned with sudden death or unexpected death. The important thing about unexpected death is that it is, well, unexpected. That means that whatever killed the person was not something that one would expect to kill him or her *today.* This can be a problem when dealing with clinicians, because we see a lot of people who are dead, but “shouldn’t” be dead. Clinicians, and others, disagree with our determination of cause of death because we invoke things that “shouldn’t” kill people.
The reason for this is that we often see the exceptions rather than the rules. I remember some years ago when I was teaching at an academic center, I signed out a death as due to community-acquired bacterial bronchopneumonia. I got a phone call from a very angry clinician telling me I was wrong. He was angry because he read my report as implying that he did not adequately treat the decedent’s pneumonia, and the patient died because of malpractice. Of course that was not the case. I asked him why he thought that, and why I was wrong. His response was that he sees people in the Emergency Department all the time with pneumonia and they *never* die. Pneumonia is treatable, and people who don’t have other vulnerabilities just don’t die of it.
I told him that he was right. Younger healthy adults with community-acquired pneumonia who receive treatment never die. Except when they do.
The difference was all about our experience. He saw tons of people with pneumonia and they all got better. I saw tons of people with pneumonia and they all died. My patients were all the exception to the rule. Even rare exceptions add up. Let’s say that only 1 in 1000 otherwise healthy patients with community-acquired pneumonia die. If you work in an ED and see 500 pneumonia patients a year, then you won’t see those deaths — even if they do die, they will die after they go home, die there, and you will likely never know. But, if you are a medical examiner in a large metropolitan jurisdiction that has 100,000 cases of pneumonia every year, you will see 100 cases a year.
Another great example is hypertensive heart disease. A question I often get from families is “Well Uncle Joe had a little bit of high blood pressure, but he’s had it for 40 years, and he felt fine. Why did he die last Thursday?” We saw that attitude in one of the clinicians who testified for the prosecution in the Chauvin trial, when he claimed that the decedent’s heart was big but “strong.” Why does a person with high blood pressure and a big, dilated, but “strong” heart die on this particular date?
The answer is that it is this combination of a vulnerable heart, a stress, and autonomic dysfunction. Hypertensive heart disease is a good example of this. The heart is a muscle. And like most muscles, the more it works the bigger it gets. When you lift weights, the extra work your arms do makes the biceps bigger. When you have high blood pressure and the heart works harder to pump blood, it gets bigger, too. As it gets bigger, it changes shape.
And that shape change is the key. The electrical conduction system of the heart runs through and along the surface of the muscle itself, and is made of specialized muscle cells that conduct electricity, called purkinje fibers. As the heart changes shape (called “remodeling”), those electrical pathways change. And as they change, they become more liable to make a mistake and result in an arrhythmia. As one study noted(1):
As a direct consequence of PCS remodeling, we found that pressure-overloaded hearts exhibited marked changes in ventricular activation patterns during normal sinus rhythm. These novel findings characterize PCS cardiomyocyte remodeling after chronic pressure overload. We identified significant hypertrophic growth accompanied by modified expression of Cx40, Cx43, and HCN4 within PCS cardiomyocytes. We found that a functional outcome of these changes is a failure of the PCS to activate the ventricular myocardium normally.
Now, of course, everybody has the occasional abnormal heartbeat, and it is almost always benign. But as the heart changes shape and the conduction system changes, it becomes more likely that an arrhythmia will happen, and more likely that it will not be benign. Of course there’s a lot more going on, but this is not a textbook on cardiac pathology. The take home message is that as the process evolves, the probability of a problem increases. But it is a stochastic process — every time your heart beats you are rolling the dice. You may not come up snake eyes today. Or tomorrow. Or for 20 years. But if you roll the dice enough times, it will happen.
Let’s add one more important thing to the process. Let’s stress the heart in a way that it has to respond quickly to some stimulus. Now, you not only have a vulnerable conduction system, but you are stressing it. For instance, let’s have you sit around being a couch potato for a month or two and then have you decide to start working out hard. Rather than ease into it, you go from zero conditioning to working until you drop. That’s a significant stress.
Now let’s add that not only is your heart not quite up to snuff, but also the part of the nervous system that controls your heart rate isn’t quite up to snuff. To remind you, the nervous system has two parallel parts, the “somatic” nervous system, and the “autonomic” nervous system. The somatic system is the one we use to move our limbs and do things with intent. However, much of our body runs without us thinking about it. We don’t “will” our heart to beat. We don’t tell our bowels to churn. We don’t tell our blood vessels to dilate and constrict. This is all taken care of in the background by the autonomic nervous system.
The autonomic nervous system has a huge effect on our heart. Our heart adjusts to changing conditions all the time. It beats faster when we exercise. It speeds up when we stand up and blood drops to our legs. It slows down when our blood pressure gets too high and speeds up when it gets too low.
Here’s the catch, though. If your heart is damaged, it sometimes can’t respond as quickly or completely as it should. And when that happens, it can lead to an arrhythmia and sudden death. How deadly can it be? There’s a great article on this published in 1993 by Willich et al (2). In it they note that there are a myriad of stresses that can cause sudden death in vulnerable people. Some examples:
The risk of sudden death increases by 2.6 times during the first couple of hours after waking up in the morning, presumably due to hormonal changes due to changing from sleeping to waking mode. The spikes are 20% higher in the winter(3).
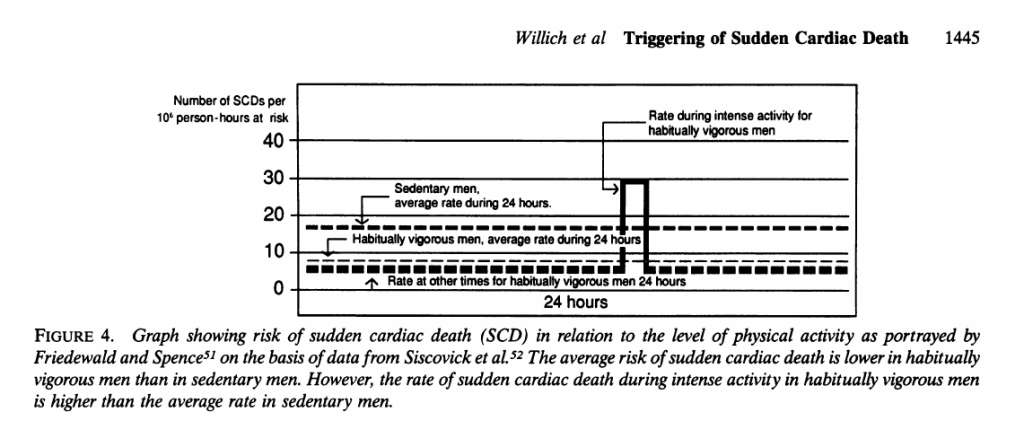
Joggers, in general, have a lower overall risk of sudden cardiac death compared to sedentary controls. However, **while jogging** , the risk is 7 times higher than that for matched sedentary people. Here’s a picture from the Willich et al. article(2):
In an older study, sudden death occurred after emotional stress six times more frequently than matched unaffected family members. The rate of sudden cardiac death predictably doubles or more after major disasters and similar events (earthquakes, floods, etc) not associated with exertion or trauma. In some cases, particularly with studies of tsunamis in the far east, these increases can last for months. During the 1991 Gulf War, the rate of sudden cardiac death doubled after Saddam Hussein shot missiles at Tel Aviv, even though the missiles didn’t kill anybody.
Another article noted(4):
Acute emotional stress can produce left ventricular contractile dysfunction, myocardial ischemia, or disturbances of cardiac rhythm. Although these abnormalities are often only transient, their consequences can be gravely damaging and sometimes fatal.
Another study found that up to 7% of sudden cardiac deaths occur in the bathroom while straining at stool. Straining at stool is technically called a “Valsava maneuver” which rapidly increases the pressure in the chest, resulting in rapid decrease in heart rate. The authors dubbed this “commode cardia” a play on the term “commotio cardia,” which, thank God, didn’t catch on. They note(5):
Our study suggests that all natural deaths that occurred on the toilet were due to commode cardia in this population. Additionally, we identified another set of deaths that occurred in the bathroom in which possibility that the decedent died on the toilet could not be excluded. Overall, the incidence of commode cardia in our population was up to 7% of all deaths attributed to cardiovascular disease in 2012. When we look at these groups, we see that these individuals are predominately older males with normal body mass indices. In approximately two-thirds of these deaths, the decedents had documented clinical histories, modifiable risk factors, and/or risk equivalents for cardiovascular disease. Some risk factors, such as smoking history, dietary habits, and activity level, were unknown. Thus, it is likely that we underestimated the percentage of decedents with underlying risk factors.
Other studies have suggested that an abnormal response to the Valsalva maneuver under testing conditions is a reasonable predictor of prognosis in patients with heart failure.
Other studies (and unfortunately I’ve lost the reference) suggest that up to 5% of deaths in an asthma attack are not due to respiratory failure but due to sudden cardiac death associated with the distress of the event.
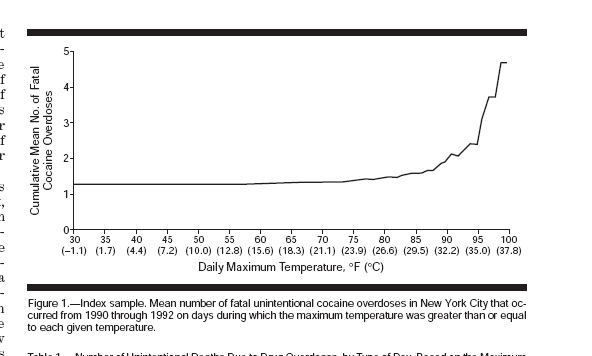
Environmental stress — heat, cold, etc. can trigger this kind of thing. Here’s a wonderful graph from an article that looked at the rate of cocaine-related deaths as a function of ambient temperature in New York City(6):
Note the sudden rise after the temperature goes above 85 degrees F. It’s not because people are taking more cocaine when it’s hot. It’s because of the combination of drug and environmental stress. And, of course, the infirm are notoriously more susceptible to heat waves and such.
Thus, it is clear that stress of any sort in a person with a vulnerable heart — even in an otherwise asymptomatic person with a big “strong” heart — can be deadly if that person rolls snake eyes. The key here, though, is that because the stress can by anything that causes a change in the autonomic nervous system, it may not be obvious what that trigger was. It could be remembering a sad event from the past, getting angry at a person driving like a jerk, a social slight, climbing the stairs quickly, whatever. Sometimes it’s clear, like getting arrested. Sometimes it’s not.
Understanding a death means understanding how these vulnerabilities and stressors work together to result in death. It is not “character assassination” to note them.
Next, how we integrate trauma as one of those insults in the determination of manner. In the next post.
- Harris BS, Baicu CF, Haghshenas N, Kasiganesan H, Scholz D, Rackley MS, Miquerol L, Gros D, Mukherjee R, O’Brien TX. Remodeling of the peripheral cardiac conduction system in response to pressure overload. Am J Physiol Heart Circ Physiol. 2012 Apr 15;302(8):H1712-25. doi: 10.1152/ajpheart.00621.2011. Epub 2012 Feb 3. PMID: 22307665; PMCID: PMC3330807
- Willich SN. Circadian variation and triggering of cardiovascular events. Vascular Medicine 1999 4(1):41-49. https://doi.org/10.1177/1358836X9900400108
- Willich SN, Maclure M, Mittleman M, Arntz HR, Muller JE. Sudden cardiac death. Support for a role in triggering in causation. Circulation. 1993 87:1442–1450 https://doi.org/10.1161/01.CIR.87.5.1442
- Ziegelstein RC. Acute Emotional Stress and Cardiac Arrhythmias. JAMA. 2007;298(3):324–329. doi:10.1001/jama.298.3.324
- Fisher-Hubbard AO, Kilak K, Diaz F, Nijiaji C, Chi P, Schmidt C. “Commode Cardia – death by Valsalva maneuver: A case series.” Journal Forens Sci 2016 61(6):1541-1545 https://doi.org/10.1111/1556-4029.13196
- Marzuk PM, Tardiff K, Leon AC, et al. Ambient Temperature and Mortality From Unintentional Cocaine Overdose. JAMA. 1998;279(22):1795–1800. doi:10.1001/jama.279.22.1795